chemotherapy
Synonyms in the broadest sense
Radiation therapy, tumor therapy, breast cancer
definition
The chemotherapy is the drug treatment of cancer (Tumor disease) that affects the whole body (systemic effect). As drugs are so-called Cytostatics (Greek from cyto= Cell and statics= stop), the aim of which is to destroy or, if this is no longer possible, to shrink the tumor. The target of chemotherapy is the division phase of the tumor cells, which they go through very often, much more often than most healthy cells, due to their uncontrolled growth. However, when chemotherapy is used, healthy cells are also damaged, which leads to the numerous inevitable Chemotherapy side effects surrender.
In order to provide the patient with the best possible therapy, chemotherapy is often combined with radiation or surgery in order to improve the outcome of the tumor treatment.
History of chemotherapy
PAUL HONEST originally re-coined 1906 the term "chemotherapy“And meant the drug treatment of an infectious disease. Today we are much more likely to name the therapeutic agents used in the event of an infection with bacteria Antibiotics and leave the term “chemotherapy” to the treatment of cancer.
How does chemotherapy work?
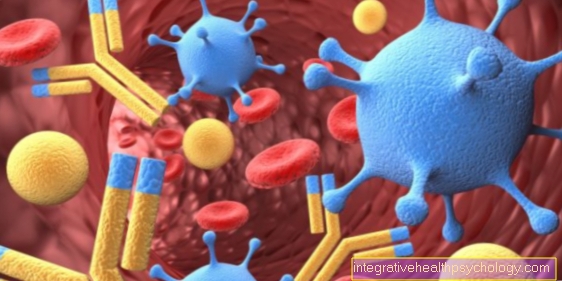
The chemotherapy or the Cytostatics prevent the cell division of the tumor cells and thus their growth. Since tumor cells divide much more often than most healthy cells in the body, they are much more sensitive to chemotherapy. This principle makes it possible to selectively combat tumor cells. In order to better understand how cytostatics work, let's take a closer look at the division cycle of a cell.
To make two cells from one cell, the entire kit of one cell must first be doubled. Both Cytoplasm with its components (enzymes, Proteins), as well as the cell nucleus with the genetic information, the DNAto be doubled. This phase is called the interphase.
The real division is mitosis. Here the DNA packed into so-called chromosomes is distributed over two cells, so that two identical daughter cells are then created. Mitosis is the main goal of the cytostatics, which want to prevent the division of the tumor cell at various points:
- The most vulnerable part of a cell is the DNA (it is the “brain of a cell”, without it nothing works). If you destroy it or disable it, the cell is practically dead. On the one hand, this can be achieved by simply smuggling in a wrong component during the production of a second, identical DNA, which leads to a break in the DNA strand arises. Tumor cells can only correct this error with difficulty or not at all, since they usually lack the repair mechanism for it. As a result, the cell triggers the self-destruction mechanism (Apoptosis) out.
- In order to separate the newly produced DNA from the old one, the cell needs an apparatus (the mitotic spindle), which some cytotoxic drugs aim to prevent division in this way. There are also cytostatics that act on the metabolism of a tumor cell instead of on division.
More details are explained under the substances used in chemotherapy!
So cytostatics intervene in the division and metabolism of cells, which, however, also take place in normal cells. Chemotherapy is therefore not only cancer-specific, i.e. it does not only attack tumor cells.
Nevertheless, mainly cancer cells are killed because they behave atypically and mainly waste their energy on division. They have forgotten their original role, such as that of skin cells, which provide protection against harmful external factors. In this context it is said that cancer cells are not differentiated enough.
However, there are also cells in our body that naturally divide often. These include the hair root cells (our hair grows constantly if we wouldn't cut it ..), the mucous membranes in the mouth and intestines and the blood-forming cells in the bone marrow! Above all, these are also attacked by chemotherapy. This results in the unfortunately unavoidable side effects.
What are the chances of success of chemotherapy?
Unfortunately, one chemotherapy give no guarantee of success because cancer is not the same as cancer. There are innumerable different ones Cancers, each of which is divided into many subspecies. Usually the histological (histological) Examination of the tumors is the only way to assign them to a specific cancer. Each type of cancer reacts differently to chemotherapy; she is either sensitiveThat means it responds to chemotherapy or it is resistantthat means the chemotherapy has no effect. Even the same cancer in two people may or may not be cured by the same chemotherapy. In order to find out which chemotherapy works for which type of cancer, various options have been tested in so-called studies over the years. Based on these study results, today's therapy standards are developed!
In principle, chemotherapy can only work if the dose, the Duration and the frequency be right. However, you cannot choose the dose as high as you want, as vital organs can be damaged. In order to increase the chance of successfully destroying the tumor cells, a combination of several is often chosen Chemotherapy drugsthat complement each other in their effect and thus cause maximum damage to the tumor cells.
With all cancer treatments it is important to talk to the doctor about the benefits, but also about the risk of the respective chemotherapy and weigh them!
Goal setting
Radiation therapy cannot always cure cancer. Nevertheless, in such cases it makes sense to undergo radiation therapy, although a cure is impossible. That is why we differentiate between different objectives:
1. Curative radiation therapy (curative = healing)
Here, cancer is supposed to be defeated by radiation therapy. It is believed that cancer patients will be cured after radiation therapy (very often this approach can be used with cancers that are spread throughout the body through the bloodstream, such as one leukemia). If you combine radiation therapy with an operation or a radiotherapy, so one still distinguishes the neoadjuvate of the adjuvant Shape:
- One speaks of one neoadjuvant Radiation therapy as one means preparatory radiation therapy that takes place before an operation. Its aim is to reduce the size of the tumor in order to facilitate the operation or to make it possible in the first place. The surgeon can now preserve as much of the healthy tissue as possible and minimize the risk of the operation.
- The adjuvant In contrast, radiation therapy (adjuvant = supportive) takes place after surgery or radiation. This is necessary because the visible after an operation tumor was removed, but it is not always 100% certain that no tumor cells have remained (R1 resection). With a subsequent radiation therapy one hopes to catch the last tumor cells and take them off. In this way one can try to prevent the tumor from breaking out again; In some cases, a remaining tumor cell may already reach a Relapse trigger. In addition, tumor cells can often be found outside the solid tumor (for example in the Lymph nodes), which one may not have reached through an operation. Since radiation therapy is a systemic therapy, it finds tumor cells everywhere in the body and destroys them.
Except before or after an operation can also be done in parallel with one Irradiation given radiation therapy.
2. Palliative radiation therapy (palliative = soothing)
In the case of a very advanced cancer disease where, in addition to the original site of the tumor (Primary tumor) already in other organs (for example in the liver) Settlements (Metastases) of the tumor are found, it is usually impossible to cure the patient (However, based on current knowledge, metastasis does not necessarily mean that there is no chance of a cure in this situation).
In these cases the chemotherapy mainly to make the remaining time as pain-free as possible for the patient. Tumor patients experience pain because the tumor is growing permanently and can therefore press on or on adjacent structures, such as in the Bone tumorbecome unstable. This can improve the quality of life and life expectancy of patients.
Ultimately, however, the decision as to which type of radiation therapy is chosen remains up to the patient. Depending on the general condition of the patient, a potentially curable tumor cannot be treated because it would be too stressful for the patient and he would like to avoid the stress of curative radiation therapy (which is much more aggressive).