Shingles
Synonyms in a broader sense
- Herpes zoster
- Zoster
English: shingles, zona, zoster, herpes zoster
General
Shingles, a viral infection, is a long-term consequence of chickenpox infection. The virus reactivates as a result of a weak immune system. However, it does not necessarily occur in all people who have already had chickenpox.

The leading symptom is the formation of blisters in a limited area of skin, which is accompanied by reddening and moderate to severe pain
Shingles is usually found on one side, rarely on both sides.
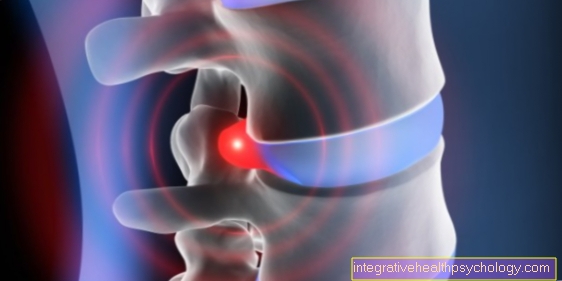
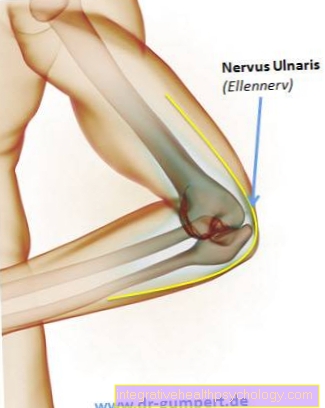
Above all, however, it is always limited to dermatomes. These are certain areas that are supplied by a cutaneous nerve. They mostly run horizontally.
Since the zoster virus is located in nerve cells, when shingles breaks out, the areas that are supplied by the nerve affected by the virus are always affected.
frequency
It is estimated that around 90% of the population is infected with the varicella zoster virus by the age of 14. You now have lifelong immunity to chickenpox.
Up to 20% of these partially immune adults develop shingles later.
Signs of shingles
The first signs of the onset of shingles are initially very unspecific.
Those affected complain of a slight feeling of weakness that is associated with fatigue, exhaustion and a slight fever.
The fever here usually only rises to values of up to 38 ° C.
After a day or two, the list of symptoms includes more specific signs such as sensitivity disorders and pain in the affected skin area.
In addition, the blistering begins and the skin begins to swell. This rash or inflammation now spreads, in most cases on one side, in a belt-shaped manner over the trunk (or other areas depending on the infestation), which is the most specific sign of the presence of shingles.
In most cases there is also nerve pain (lat .: neuralgia) of the affected nerve, which is accompanied by severe itching. This nerve pain is felt by many to be stabbing and painful and should be treated with adequate pain therapy.
This is discussed in more detail in the section What helps against pain in shingles.
Read more on the topic: pain in the back
Is shingles contagious?
The viruses that cause shingles are the same as those of chickenpox.
For infection with these viruses, direct skin contact with the contents of the vesicle is necessary (smear infection).
If the vesicles are encrusted, there is no longer any risk of virus transmission.
However, it is not possible to contract shingles directly: it can only lead to an outbreak of chickenpox - and that only affects people who have not yet had chickenpox or are not vaccinated.
As a rule, chickenpox develops after about 2 weeks, in individual cases after one or only after 4 weeks. If you have already had chickenpox or have been vaccinated against it, there is consequently no risk of infection from people who have shingles.
Shingles itself is an endogenous infection. This means that the chickenpox virus is reactivated at some point when the immune system becomes weak.
Read more on the topic: Is Shingles Contagious?
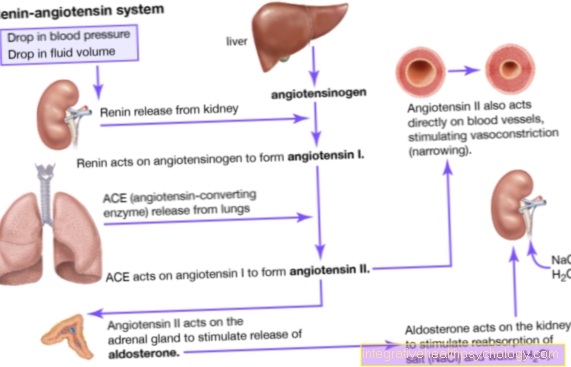
root cause

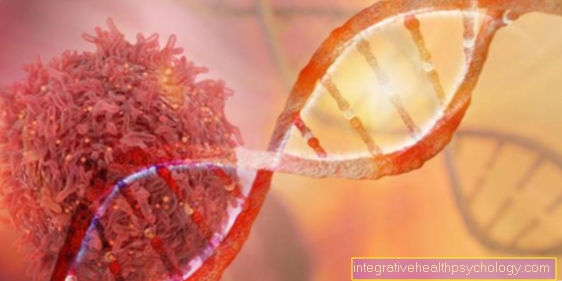
Shingles is caused by the varicella zoster virus.
When infected with this virus for the first time, the clinical picture of varicella, chickenpox, occurs.
Usually, chickenpox is a one-off disease in childhood and adolescence. Chickenpox is transmitted through droplet infection (e.g. cough). However, the viruses remain in the body even after healing.
They withdraw along the nerve fibers into the spinal ganglia. Spinal ganglia are switching points in the central nervous system. They are located near the spinal cord.
If the immune system is weakened, the virus can reactivate. This condition is called shingles. Sun exposure and stress can also promote zoster.
Herpes zoster infection is only possible through the transmission of the virus-containing vesicle contents, but it is minimal. Only people who have not yet had chickenpox and are not vaccinated can become infected. These people would get chickenpox, not shingles.
There is no direct infection with shingles. This means that someone who has shingles cannot infect anyone with shingles.
Read more on the topic: Causes of Shingles
Can shingles be caused by stress?
Stress is definitely one of the risk factors for the outbreak of shingles.
Various factors such as stress can now reactivate the viruses. The result is the development of shingles. To what extent stress leads to an activation of the virus is not yet understood in detail. It is currently assumed that stress weakens the immune system, which means that the virus can no longer be kept in check and that it is activated again.
Other risk factors are
- an immune deficiency,
- major trauma
- and intense UV radiation.
Read more on the topic: Stress as a cause of shingles
Can shingles be an indication of HIV?
Many different factors can be responsible for the outbreak of shingles. When asked why the varicella-zoster viruses are sometimes inactive in a body for years and are suddenly activated and cause shingles, science is currently unable to give an exact answer. However, there are some known risk factors that make shingles more likely to break out. In addition to stress and major injuries, these also include an existing immune deficiency. There are a variety of reasons that can cause immunodeficiency. One of these reasons could be the presence of HIV or AIDS. However, it is wrong to conclude that shingles is a clear indication of the presence of HIV.
Read more on the topic: Symptoms of HIV
Symptoms of Shingles
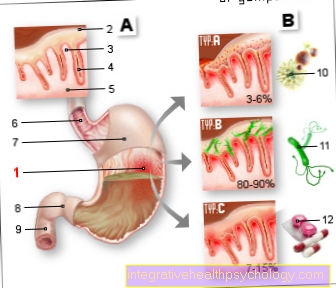
Herpes zoster (shingles) is preferred in older people or in immune deficiencies (e.g. AIDS, leukemia). The infection is usually limited to one or more dermatomes (the area where a nerve spreads). In contrast to chickenpox, which affects the entire body, shingles is localized.
The affected skin segments are characterized by very painful and grouped vesicles on a reddened background. The vesicles contain virus-containing fluid.
After a few days of the painful phase, several inflammatory foci with clear vesicles form. 2-7 days later, the vesicles are cloudy and yellowish, the reddening subsides and the skin becomes pustular and bleeding. Now the dehydration begins. After 2-3 weeks the vesicles will heal and have left pale scars.
In addition to very severe pain with shingles, it can also lead to a fever.
Shingles pain
Characteristic of a herpes zoster infection or shingles is the occurrence of specific pain in a certain body / skin area that is supplied by a nerve of the affected ganglion (= accumulation of nerve cell bodies). The pain often begins several days before the actual, classic skin rash of shingles breaks out and is accompanied by itching in this area.
In the initial acute phase, there is predominantly dull, burning pain, which can often be aggravated by movements. It is triggered by the fact that the infection with the herpes zoster virus leads to the release of chemical substances which the pain receptors (Nociceptors) irritate the affected area. In medical terminology, one therefore speaks of nociceptive pain.
In the further course there is a neuropathic pain, which is a pain of the nerves themselves. Its origin is due to the viruses that attack the nerves and spread through their pathways. This sharp shooting pain can be triggered during the entire phase of the disease, often by light touch. Sometimes the pain is accompanied by a tingling sensation or, in exceptional cases, by symptoms of paralysis.
In some sufferers, the neuropathic pain persists beyond the actual course of the disease, in this case one speaks of post-zoster neuralgia.
Read more on the topic: Burning skin - what to do?
Course of shingles
The course of shingles is generally divided into two phases,
- the Prodromal phase (German: precursor phase)
- and the Acute phase.
The first symptoms of shingles are initially very unspecific and consist of
- general exhaustion,
- Fatigue,
- Body aches
- and fever.
Only after the start of the acute phase do the disease-specific symptoms develop, which can now only be treated symptomatically. These symptoms include the formation of blisters, reddening and severe pain in the affected skin area. The affected skin area is usually described as belt-shaped, since only the skin area that is sensitively supplied by the affected nerve shows symptoms.
Usually, abnormal sensations or numbness in the skin area are also reported in the course of the disease.
After approx. 4-5 days, the vesicles filled with clear liquid burst and a wound crust begins to form. 14 days after the onset of symptoms, the shingles will have healed in most patients. This healing process can be accelerated by an appropriate therapy with skin ointments.
Read about this too: How long does shingles last?
diagnosis
Important for the diagnosis of shingles are the typical and obvious symptoms and symptoms.
Extreme pain drives the patient to the doctor and the typical distribution of the blisters and reddening is evident.
A pathogen can also be detected. Both antigen (i.e. the virus (Herpres zoster) per se), as well antibody (against the body through the body's immune response to the virus). Antibodies are, however, already formed during the first infection, i.e. chickenpox, and are therefore not well suited for diagnosing zoster / shingles.
Is there shingles without the typical blisters?
In rare cases, shingles may be present without blisters or reddening.
This phenomenon is called 'Zoster sine herpete' designated.
Such a manifestation makes the diagnosis more difficult, since the other symptoms such as nerve pain are not very specific for shingles.
However, the basic course of shingles without a rash or blisters is similar to normal. Initially, patients often report tiredness and fatigue that are accompanied by a fever.
There are also abnormal sensations in the skin area that is sensitively supplied by the affected nerves.
After one or two days, the feeling of discomfort changes to a nerve pain, a so-called one neuralgia, which is usually accompanied by pronounced itching.
In this case, antigen detection or a virus culture is required to confirm the diagnosis of shingles, as the specific symptoms of shingles are not present. The therapy for this type of shingles only consists of relieving nerve pain until the shingles subsides.
Differential diagnosis / exclusion disease
At the beginning Zoster / shingles must be considered to distinguish the following other diseases:
- Pleurisy (= pleurisy)
- pinched nerve
- Muscle inflammation
- Herpes simplex skin infection
Pictures of those affected


Which doctor treats shingles?
If the first symptoms of shingles appear in a patient, he is well advised to first visit his family doctor.
If the typical symptoms are present, the doctor can usually diagnose shingles relatively quickly and begin appropriate therapy with antivirals and usually a zinc ointment.
In most cases this is a good treatment for the symptoms of shingles.
After a week you should visit your family doctor again to check the progress. However, if the course of the disease is very severe or if the disease is in the area of the eyes or ears, which can be associated with functional failures, it is advisable to go to the hospital for further clarification.
therapy
The aim of treating shingles is always to alleviate the existing symptoms and to cure them as quickly as possible; a complete elimination of the virus pathogen is not possible. In addition, drug therapy should be started as soon as possible after the first suspicion in order to avoid chronic complications. The first focus of drug therapy is antiviral therapy, which is supposed to inhibit the spread of the herpes zoster virus and cause faster healing. In most cases, this therapy is also combined with the administration of painkillers and ointments to the affected areas.
Shingles caused by herpes zoster requires antiviral treatment. Usually Aciclovir® is used. This can be taken orally, i.e. in tablet form, or i.v. (intravenous) by infusion. Zostex® (with the active ingredient brivudine) can also be used as an oral therapy. Acyclovir and brivudine belong to the group of antivirals. These are active ingredients that specifically counteract the growth and reproduction of viruses. They inhibit the build-up of virus DNA.
Learn more at: Zostex®
Other antiviral drugs include valaciclovir and famciclovir. Ibuprofen or ASA (acetylsalicylic acid) are the main pain relievers. For the local treatment of the blisters, zinc ointments are also prescribed in most cases, which cause the blisters to dry out and relieve the existing itching.
Shingles can also be improved with homeopathic substances (please refer: Shingles and homeopathy).
Also read our article about Shingles medication!
Zinc ointment
The use of zinc ointment is part of the standard therapy for shingles.
For one, it has included zinc oxide antiseptic effect, which prevents further spread of shingles and bacterial colonization.
In addition, certain ingredients in the zinc ointment have a strong water-drawing effect, which causes the blisters to dry out. On the one hand, this improves the course of the disease and, at the same time, enormously alleviates the severe itching.
The cream should best be applied to the affected skin area 3 times a day. In addition, it then takes about half an hour to dry out well and remove the liquid from the bubbles. Thorough and regular use can have a strong positive influence on the course of the disease.
What helps against the pain?

For those affected, shingles is usually associated with severe nerve pain, a so-called neuralgia, which in rare cases can persist even after the disease has subsided.
When treated with antivirals (drugs that inhibit the growth of the virus), the pain usually disappears very quickly.
If this is not the case, targeted pain therapy can also be carried out.
According to current studies, Lyrica®, a drug that acts directly on the painful nerves, is particularly suitable for typical zoster pains.
Usually used for mild pain
- Ibuprofen,
- Paracetamol
- and acetylsalicylic acid (ASA, Aspirin®)
If the pain cannot be adequately relieved by these medications, one can either fall back on the aforementioned Lyrica®, or one must resort to stronger remedies such as tilidine, which already belong to the group of low-potency opioids.
As a rule, however, most of the pain caused by shingles can be treated well with the lighter, non-opioid pain relievers.
What can you do about itching?
For those affected, if there is no severe nerve pain, treatment of the severe itching is usually the focus of attention.
Probably the best known and most frequently used treatment is the zinc ointment. This has an antiseptic effect and helps to dry out the blisters, which leads to a significant reduction in the itching.
The ointment should be applied directly to the blisters.
We strongly advise against scratching the blisters as it increases the risk of a second infection in other parts of the body.
If the itching cannot be treated adequately as a result, local therapy can be provided after consulting a doctor Lidocaine, a local anesthetic.
Homeopathic therapy for shingles
In the treatment of shingles, homeopathic agents can be used to relieve symptoms. However, they should be used in parallel to conventional medical therapy and not replace it. It is not advisable to independently discontinue prescribed medication.
Well-known homeopathic medicines in the therapy of shingles are:
- Mezereum (D6),
- Ranunculus bulbosus (D6)
- and Arsenicum album (D12).
These active ingredients primarily help in the therapy of pain that can occur when touching, moving and often at night.
Read more about this at: Homeopathy for shingles
Home remedies for shingles

In addition to drug therapy, there is also the option of treating shingles in parallel with home remedies.
The use of cabbage is very well known. The inner, still fresh leaves of this are used. It is best to run a rolling pin over the leaves so that the liquid can escape.
These leaves can now be put on the inflamed and blistered skin area with a poultice. In addition to the cooling and moisturizing effect, it is also assumed that those contained in the liquid Antioxidants Have a decongestant effect on the blisters and promote the regeneration of the skin.
Some people are also convinced of the use of lemon balm. The leaves are used to boil a tea, let it cool down and then dab the affected skin area.
It is assumed that lemon balm has an antiviral effect, which helps the body fight the virus.
A paste made from water and baking soda is also often recommended to dry out the skin, which causes the blisters to recede and thus relieve itching. Home remedies for existing nerve pain, neuralgia, are very controversial and are rarely recommended by doctors.
Can you drink alcohol if you are being treated for shingles?
During the therapy of shingles one should refrain from consuming alcohol.
This weakens the immune system and thus has a bad influence on the course of the disease.
The same applies to the consumption of nicotine or other drugs. Alcohol also makes some drugs less effective. Thus, with appropriate consumption, the antivirals and analgesics cannot work adequately and the healing of shingles is delayed.
We therefore advise against the consumption of alcohol or other drugs as long as the shingles has not completely healed.
Complications of shingles
Depending on the affected skin segment, other organs can also be involved Shingles be affected. Is that for example face infested, there is a risk of involvement of the eyes (Zoster ophthalmicus) with possible corneal damage.
It can also damage the Ear (Zoster oticus) with possible paralysis of the face (approx. 60%).
Another complication arises from immunodeficiency. In immune-compromised patients, for example, it can lead to a generalize herpes zoster come. The spread of the skin changes beyond the dermatomes creates an image that is reminiscent of chickenpox. Here the pustules are distributed over the entire body. Furthermore, organ involvement can occur (lung infection or inflammation of the liver).
However, the most feared complication is this postherpetic neuralgia. These are piercing and burning Persistent pain and Attacks of painwhich often only appear over the years. The pain is caused by the Involvement of the nerves.
Post-zoster neuralgia

Post-herpetic neuralgia or post-herpetic neuralgia is a nerve pain that persists even after shingles has completely subsided. Hypersensitization (increased sensitivity) of the pain fibers in the affected area is suspected to be the cause, which leads to persistent, increased pain sensitivity.
According to the statistics, it affects around 10-15% of patients who were previously ill with a herpes zoster infection. The likelihood of suffering from post-herpes zoster neuralgia increases with age. It is most common on the face.
The pain is observed no earlier than four weeks after the shingles has subsided and is described as a dull, burning pain that is accompanied by sharp, shooting attacks of pain. In addition, there may be an oversensitivity of the skin area to touch, painful paresthesia and increased sensitivity to pain.
Postherpetic neuralgia can be treated by administering antidepressants (e.g. amitriptyline), anticonvulsants (e.g. gabapentin), local anesthetic creams or gels, or by performing a sympathetic blockade.
Every second person affected will recover on their own within a year, and every fourth patient will recover from the postherpetic neuralgia. If the pain persists for more than a year, a complete regression can unfortunately only be viewed as very unlikely. Treatment of the herpes zoster infection initiated at an early stage can counteract the development of post-herpes neuralgia.
Get more targeted information about Post-zoster neuralgia.
forecast
At immune strong Patient is the forecast the shingles Well. Two thirds of the diseases heal without consequences. The long-lasting ones pose a therapeutic problem postherpetic neuralgia (Nerve pain). It occurs at about a tenth of the patients and can take months to years.
At immunocompromised people however, the course of shingles is severe and the Forecast bad. Fatal forms and complications occur. Early or timely antiviral therapy significantly improves the prognosis.
Can shingles be fatal?
In principle, shingles caused by the herpes zoster virus is not fatal.
In the majority of patients, the disease takes a normal course and is healed after about 2 weeks.
In rare cases, however, serious complications in the course of the disease or secondary diseases can lead to life-threatening situations.
This is especially the case with patients who have previously had a pronounced immune deficiency. In addition to congenital weaknesses in the immune system, this can be caused by AIDS or leukemia.
In these patients there is one all over the body generalized Blistering. The virus can spread to internal organs or the entire nervous system and cause serious complications. In such a case one speaks of a Generalized herpeswhich can be fatal without treatment. However, this pronounced clinical picture is rare and only occurs in people with pre-existing immune disorders. Therefore, a clarification must be carried out when it occurs.
In addition, there is an increased risk for a due to the open skin areas in the affected area Secondary infection with bacteria. For these reasons, patients with a pronounced immune deficiency and existing shingles should be checked frequently in the course of the disease in order to rule out possible complications.
Duration
After the chickenpox or chickenpox symptoms have subsided, the virus remains in the body. If the immune system is severely weakened, e.g. due to extreme stress or illness, the virus can break out again.
Shingles usually heals after about 2-3 weeks. This is at least true for otherwise healthy people. If the patient is severely immunocompromised, the shingles can last longer. If previous illnesses are known that weaken the immune system, you should definitely consult your doctor in order not to unnecessarily prolong the healing phase of the shingles.
Read more on the topic: How long does shingles last?
How long is the incubation period for shingles?
Since the pathogen causing shingles is already present in the person's body and only needs to be reactivated, it is difficult to determine the exact incubation time (time between infection and the onset of the disease) for shingles.
Many years can pass between the initial infection, which manifests itself in the form of chickenpox, and reactivation of the virus, which is why most patients do not develop shingles until they are older. If reactivation occurs, the typical symptoms, such as the rash and blistering, develop completely within the next five days.
Read more on the topic: Shingles incubation period
prophylaxis

Since shingles can only break out if there has already been an infection with the varicella zoster virus, a vaccination against chickenpox is quite suitable as a prophylaxis. This vaccination is one of the standard vaccinations for children and adolescents. Women of childbearing potential should always be vaccinated, as a possible infection during pregnancy will harm the child.
No vaccination should be given during pregnancy. No vaccination against shingles should be carried out in immunocompromised people, as there is a risk of so-called “vaccine varicella”, ie an outbreak of the disease (chickenpox) due to the vaccination.
You might also be interested in this: Zostavax® vaccination against shingles
How long is shingles contagious?
Transmission usually takes place via body fluids, which is why shingles is one of the so-called smear infections. For this reason, it can be said that shingles is contagious as long as wound fluid leaks from the blood cells and the skin is infected.
Furthermore, it should be noted that shingles must always be preceded by chickenpox disease. Years often pass between these two diseases, but they are caused by the same pathogen. If a patient with existing shingles infects another person who has never had chickenpox, he or she will first get chickenpox and not develop shingles.
In patients who have already been infected with chickenpox, if they are infected with the herpes zoster virus, there is an increased risk of the viruses still present in the body being reactivated and shingles developing. You should be very careful not to come into direct contact with the vesicle fluid, as it can be potentially contagious. In addition, one should pay attention to adequate hand hygiene.
Please also read: How contagious is shingles?
Shingles during pregnancy
During pregnancy, the pregnant woman should avoid close contact with people with shingles.
If a mother suffers from shingles during her pregnancy, there is basically no significant risk for the unborn child if she is immune to the varicella virus.
However, if the pregnant woman has no immunity because she has not been vaccinated or has not yet had chickenpox, there is a risk that contact with shingles will lead to chickenpox in the mother.
The first occurrence of chickenpox during pregnancy is rare but severe.
The unborn child is infected in around a quarter of all cases. This can be without consequences, but it can lead to serious malformations in the child and even death, especially if the mother is seriously ill.
In certain cases, for example if the spouse suffers from shingles and the mother-to-be has no chickenpox and is not vaccinated, so-called post-exposure prophylaxis is recommended. Antibodies are injected to "catch" the pathogens. In this way, the onset of the disease can be prevented or at least the course can be weakened.
Read more on this topic at: Shingles in pregnancy
Shingles in children
Even in children, shingles can only occur after they have been through it Chickenpox infection occur. Overall, shingles is common in children, especially in the first 10 years of life, rather seldom.
If a child has contact with someone who has shingles and has not yet had chickenpox or vaccination, the chickenpox disease can be transmitted through this. The course and treatment of shingles in children differs depending on the status of the person's immune system. If the functioning of the immune system is intact, shingles is usually harmless and self-limiting. This means that no specific therapy for shingles is required and the disease heals on its own.
In this case, symptomatic therapy is carried out:
If you are in pain, taking Pain medication or the application numbing ointments help. Against the itching can also be one Itch relieving lotion can be used. Since the chickenpox is at risk of bacterial infection by constantly scratching it, this risk is also reduced by using a special anti-pruritic substance.
At Children without an intact function of the immune system, for example at chemotherapy or one HIV infection, shingles can have a serious course that can lead to death. Therefore, in a children's clinic, the child should receive an anti-virus agent in the form of infusions.
Shingles on different parts of the body
Shingles on the face and head
If the viruses reactivate, they can attack the adjacent nerves and cause the typical symptoms of shingles. In the head area, the Opthalmic nerve and the Facial nerve be affected, each of which is associated with different characteristics. What these different manifestations have in common is the typical reddening and blistering in the affected skin area.
Due to the numerous sensitive structures, shingles on the face is relatively often associated with complications, and almost all structures can be affected by inflammation.
Is the Opthalmic nerve affected, the top branch of the Trigeminal nerve, symptoms mainly occur in the area of the eyes; photophobia, tearing, redness and swelling can occur. If the inflammation spreads to the cornea, it can scar, which in the worst case can lead to blindness and should therefore be treated quickly and adequately. Conjunctivitis is common.
In rare cases, the auditory nerve, Cochlear nerve, or the equilibrium nerve, Vestibular nerve, to be affected. Here, too, inflammation leads to corresponding failures in sensory perception, i.e. to hearing or balance problems. This is called Herpes zoster oticus designated.
Shingles affects the Facial nervethat runs through the ear, the temporary, mostly one-sided paralysis of the facial muscles and the loss of taste are the main focus of the symptoms.
In general, there is an increased risk of shingles on the face, and once the shingles has subsided, one postherpetic neuralgia to get. These are pains that are caused by the irritated nerve itself and are often not easy to treat. As on other parts of the body, shingles can also cause scars on the face. It is important that this risk can be reduced by starting therapy early.
Read more on the topic: Shingles on the face
Shingles of the eye

Shingles of the eye is very uncomfortable for those affected and, in severe cases, can lead to impaired vision in the affected eye.
The inflammation can affect all structures of the eye. In most cases there is inflammation of the conjunctiva (Conjunctivitis).
If the course is severe, the inflammation can also affect the retina, which results in a partial to complete malfunction. However, only in a few cases are these perceptual disorders permanent.
Furthermore, the inflammation and the associated accumulation of fluid can lead to an increase in intraocular pressure, which should be checked by an ophthalmologist.
A long-term complication of shingles of the eye is that the risk for what is called Post-zoster neuralgia higher than at other locations.
A Post-zoster neuralgia describes a nerve pain that persists after the disease and that originates from the affected nerve and can be extremely uncomfortable for the patient. It also often leads to a severe headache sensation.
For these reasons, it is advisable to treat shingles in the head area with virus-inhibiting drugs (Antivirals) to treat. This also prevents the development of post-zoster neuralgia.
Shingles on the ear
Shingles on the ear is called Herpes zoster oticus designated. Shingles on the ear is rare compared to other locations.
In addition to the well-known and typical symptoms of shingles such as:
- Blistering on the ear and in the external ear canal,
- fever
- and severe itching
This can lead to severe functional impairments in the area of the face.
These functional failures can affect hearing, the sense of balance, the sense of taste and the movement of the facial muscles.
This wide range of failures is due to the fact that the nerves responsible for these functions run very close together and so an inflammation of one nerve can spread to the other very quickly. In order to avoid permanent damage, patients with shingles should consult a doctor as soon as possible so that drug therapy can be started. As with all types of shingles on the head, this is recommended to prevent long-term effects.
Read more on the topic: Herpes zoster oticus
Shingles on the neck
A Shingles on the neck usually runs similar to the rest of the body. However, the proximity to the face is problematic.
For example, it can easily infest the Oral mucosa come. This manifests itself in numerous painful and easily bursting blisters. Often, food intake is hardly possible due to pain.
Due to the course of the nerves, a Shingles on the neck also to one Paralysis of the facial muscles to lead. Normally, this regresses completely over time, but in individual cases the person concerned also retains consequential damage, including Speech disorders can count.
A complication that is not uncommon with shingles of the neck is that Post-zoster neuralgia (Nerve pain). These are expressed as short or piercing attacks of pain Pain when touching the affected area. Older people aged 60 and over are particularly affected, although the pain sometimes only occurs after the illness has ended. For this reason, if pain in the face and / or sore throat occurs after shingles, it is essential to report to the doctor treating you that you previously had shingles. This is the only way for the doctor to know the cause of the pain and how to treat it correctly.
Shingles on the leg
Shingles on the leg is the third most common localization and occurs when Nerves supplying the legare infected by the varicella zoster virus. The nerve root des Lumbar nerve L3 affected. The associated Dermatome, i.e. the area of skin it supplies, stretches over the thigh to the inside of the knee in most people. If both legs are affected in rare cases, one speaks of the so-called Zoster duplex.
The symptoms correspond to typical shingles and can be identified as such by the doctor through a visual diagnosis. The therapy takes place through the administration of antivirals, painkillers and antibiotics.
Complications can occur if a bacterial infection also occurs or the affected skin dies (necrosis). Long-term consequences can be persistent nerve pain (zoster neuralgia), hypersensitivity to the affected skin areas or scarring.
Read more about the topic here: Shingles on the leg
Shingles on the back
Shingles on the back is relatively common when compared to other areas of the body.
In 60% of cases of shingles, areas of the back are affected.
As a rule, however, it only spreads on one side, only very rarely does it encompass the entire body in a belt-shaped manner.
In addition, in most cases the skin areas above the lumbar vertebrae are affected, from which the inflammation and the formation of blisters spread to the front.
For those affected, shingles on the back is very uncomfortable, especially at night, as lying on the back is associated with pain.
In addition, the vesicles can burst and wound fluid can leak out.
For these reasons, most patients with shingles on their back sleep on their stomach. On the back, more often than elsewhere, the itching that is always present is perceived by those affected as severe pain.
Shingles on the stomach
In almost all cases, shingles spreads in the area of the abdomen and chest with the typical pattern. The pattern of spread is usually one-sided and belt-shaped, only in rare cases does the disease affect both halves of the body. The affected skin area shows sensory disturbances, blisters, reddening with swelling and severe nerve pain. If the shingles occurs in the area of the belly button, it can be very annoying for those affected because the blisters can be compressed and burst when you sit down. This also makes it more difficult for the blisters to dry out, as the affected skin area cannot be kept dry at all times.







.jpg)