Pain at the entrance to the vagina
definition
Pain at the vaginal entrance is not unknown to many women. The fear of serious illnesses and restrictions in everyday life, and especially in relationships, are often very stressful. Pain is the symptom of many causes, most of which are easily treatable. The genital area is very sensitive because there are many nerve endings here. Even the smallest change can lead to discomfort.

causes
There are many causes of pain at the vaginal entrance. Short-term pain can occur after intense or frequent intercourse due to irritation. Intensive cleaning with aggressive care products can also irritate the vagina.
Long-lasting pain can be triggered by inflammation in the genital area. Often there is one Bartholinitis, an inflammation of the duct of the Bartholin's gland. Other infections with fungi, viruses, bacteria or parasites can also trigger pain. These diseases are often sexually transmitted diseases.
In rarer cases, benign and malignant changes can also be the cause of pain. Vulvar and vaginal carcinoma and its precursors, vulvar / vaginal intraepithelial neoplasia (VIN / VAIN) can trigger chronic pain, especially at an advanced stage.
Natural processes can also result in pain. During menopause, but also outside of it, vaginal dryness can occur in many women, which can be painful in some cases. A so far rare diagnosis is the so-called vulvodynia, chronic pain in the genital area for which there are no obvious physical causes.
Read more on the topic: Vaginal infection
Bartholinitis as a cause of vaginal entrance pain
Bartholinitis, an infection of the duct of the Bartholin gland, can be triggered by various germs. The most common are bacteria like Staphylococci. A purulent inflammation develops, in which the surrounding tissue swells.
The swelling is usually one-sided in the back third of the labia and can be the size of a chicken egg. It usually causes severe pain. The surrounding tissue can also melt down, creating an abscess, a cavity filled with pus.
Read more on the topic: Bartholinitis
Pain at the entrance to the vagina during pregnancy
Varicose veins can increase during pregnancy (Varices) come from the vagina. Due to the pressure of the growing uterus and more flexible veins, these can strengthen or form more easily. These varices are recognizable as bluish vessels and can be itchy or painful.
Pain at the entrance to the vagina during sexual intercourse
Pain during intercourse (Dyspareunia) can have both psychological and physical causes.
Stress in particular often leads to tense pelvic muscles and a vagina that is too dry. Inflammation, irritation or allergies in the genital area can also lead to pain during sexual intercourse. Especially during breastfeeding and menopause, the vagina is often dry and can be painful, especially during intercourse.
A tight hymen can lead to pain, especially during the first sexual act.
You might also be interested in:
- Pain during sexual intercourse
- hymen
Vaginal dryness as a cause of pain at the entrance to the vagina
Both physical and psychological causes can trigger vaginal dryness. Women of any age can be affected. In addition to pain, especially during sexual intercourse, vaginal dryness often leads to itching, burning of the skin and burning sensation when urinating. In addition, vaginal dryness makes it easier for pathogens to colonize the vagina and can thus lead to unpleasant infections.
A common cause is a lack of estrogen, which occurs particularly during menopause. But even after pregnancy and while breastfeeding, through certain medications, radiation or chemotherapy, and through stress, the body's estrogen production can decrease.
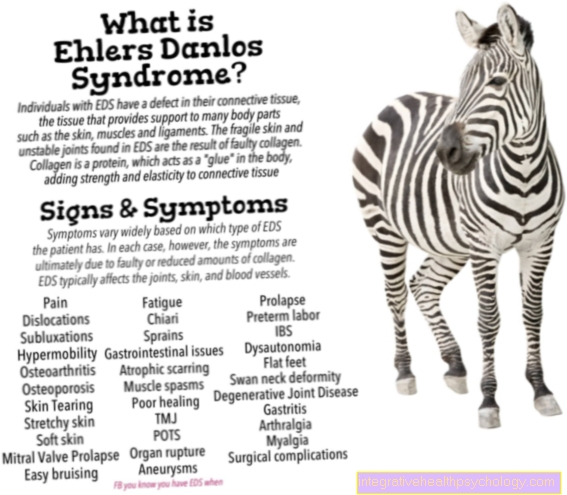
Estrogen plays an important role in the production of vaginal fluid, which keeps the vagina moist and protects it from pathogens. In addition, certain diseases such as diabetes, high blood pressure and autoimmune diseases can cause a dry vagina. Certain contraceptives, the consumption of alcohol, smoking and excessive hygiene of the genital area with aggressive soaps and creams can also trigger or intensify dryness by changing the pH value of the vagina.
You might also be interested in: Vaginal dryness
Fungal infection as a cause of vaginal entrance pain
Vaginal fungal infections (Genital thrush) are a common condition in women. The most common pathogen is Candida albicans, which is why one calls it a Candidiasis speaks. Symptoms of a genital indoor are itching and burning of the vagina, whitish evidence, reddened vaginal skin, and a crumbly discharge.
Candida fungi colonize the skin or mucous membranes in small numbers in many people without causing symptoms. Infection only occurs when the immune system is disturbed. This can be the case due to diseases such as AIDS, cancer, diabetes or alcoholism. Hormonal changes during pregnancy can also disrupt the immune system.
Drugs are also common causes. Antibiotics can disturb the balance between fungi and bacteria and lead to overgrowth of fungi. Immunosuppressants, cortisone or chemotherapy, on the other hand, directly weaken the immune system and increase susceptibility.
Read more on the topic: Vaginal fungus
diagnosis
A combination of a medical consultation and a gynecological examination with swabs of the genital area is necessary for the diagnosis. In the conversation, particular questions are asked about current complaints.
Bartholinitis is usually a visual diagnosis as the symptoms are very typical. Inflammation of the genital area is diagnosed with a smear. Above all, it is checked which pathogen is causing the symptoms. Benign and malignant changes can be detected by taking a sample of the changed region and then examining it under the microscope.
Varicose veins and vaginal dryness are also visual diagnoses.
To rule out an estrogen deficiency, blood must be drawn and the amount of hormones checked. The Vulvodynia is a diagnosis of exclusion after no cause has been found gynecologically, dermatologically, neurologically and possibly also orthopedically.
Accompanying symptoms of pain at the vaginal entrance
Just like the causes, the accompanying symptoms can vary. In bartholinitis, abscesses can lead to other general signs of inflammation such as reddening and warming of the skin. Inflammation in the vaginal area often causes unspecific itching, burning, redness, pain when urinating and / or sexual intercourse and, if necessary, changes in the vaginal discharge.
The inguinal lymph nodes may also be enlarged. Depending on the pathogen, typical symptoms such as whitish deposits with a fungal infection or blisters with a herpes virus infection can occur.
Benign changes can lead to skin changes such as whitish, shiny skin and reddening of the skin, itching, burning irritation, sensation of wetness, warts and discomfort during sexual intercourse.
Malignant changes can lead to itching long before visible changes. Burning and swelling can also occur. Dark skin changes and whitish mucous membranes are another sign of malignant changes.
A dry and irritated vagina is also noticeable through itching, burning and problems with intercourse. In addition to pain, varicose veins also often experience itching.
You might also be interested in: Swelling in the vaginal entrance
Therapy for pain at the entrance to the vagina
Irritation of the vagina from aggressive care products can be prevented by using milder care products or only lukewarm water for cleaning.
For bartholinitis, the therapy of choice is what is known as Marsupialization. A small incision is made in the swelling, the edges of the Bartholin glands are folded outwards and sutured to the labia. If there is an abscess, the pus is drained and, if necessary, tested for pathogens.
In the case of inflammation in the vaginal area, the therapy depends on the particular pathogen. For herpes infections, antivirals such as Acyclovir Used locally or in severe cases in tablet form, fungal infections are treated with antimycotics such as Clotrimazole treated.
In the case of bacterial inflammation, the choice falls on antibiotics such as Metronidazole in tablet or ointment form. If necessary, the sexual partner must also be treated if it is a matter of sexually transmitted diseases.
Depending on the type of benign changes, symptomatic corticosteroid creams can be used. Warts are first treated with the antiviral drug Imiquimod then treated with the help of CO2 laser, cold therapy (Cryotherapy) or a noose.
When treating malignant changes, therapy depends on the stage. In preliminary stages, removal by laser or surgery is performed. In the case of carcinomas, these are cut out as widely as possible and, depending on the location of the tumor, either radio or chemotherapy takes place.
In the case of vaginal dryness due to a lack of estrogen, creams, suppositories or gels that are applied topically help in most cases.
In more severe cases, for example during the menopause, when other symptoms arise, hormone therapy with progestin-estrogen preparations can be used.
There is as yet no causal therapy for the treatment of vulvodynia. Creams with estrogens or anesthetics can be applied locally and pain killers can be taken for chronic pain. Pelvic floor biofeedback and neuromodulation are also used in these cases.
Varicose veins during pregnancy usually go away or improve on their own after giving birth. In order to alleviate the current symptoms, cooling or padding sanitary towels can be helpful.
You might also be interested in: Abscess in the genital area
Duration of pain at the entrance to the vagina
Depending on the cause, the duration of the pain is difficult to estimate.
Small injuries and irritations can heal quickly and cause pain only for a short time. Inflammations often develop within a few days, malignant changes can develop over years and often do not trigger any symptoms, especially in the beginning.
Vulvodynia is a chronic pain disorder. The pain often disappears as soon as therapy is successful. In the case of varicose veins due to pregnancy, these usually recede after the birth.