Tooth extraction
definition
Tooth extraction is the non-surgical removal of a tooth from the oral cavity, i.e. the dentist does not have to make an incision in the mucous membrane with a scalpel.
Colloquially, the whole thing is also called pulling a tooth.

Causes - an overview
Tooth extractions are the last resort when everything else has been tried.
The dentist will always try to save the tooth in question first and only use the forceps when all other means of therapy have been exhausted. Reasons for tooth extraction can be:
- Deep caries with extensive destruction of the hard tooth substance (cannot be filled and cannot be crowned)
- badly chipped teeth
- broken root
- severe inflammation of the tooth root which has made all other attempts at treatment unsuccessful
- Lack of space in the jaw (jaw crowding)
- very high degree of loosening (tooth can be moved with the tongue)
Causes in detail
Tooth extraction is absolutely necessary if the tooth has previously been so badly damaged by caries that fillings cannot be made and a crown cannot be anchored.
In order to be able to securely attach a crown to a tooth, you need enough remaining tooth and the caries must not reach too deep into the gums.
If the crown is deeply infected, it can no longer be ensured that no bacteria are trapped under the crown when the crown is attached. These can destroy the tooth from the outside inwards without being noticed.
Even if the tooth root has broken apart or has a longitudinal crack, this tooth can only be removed. The root holds the tooth firmly in the jawbone and ensures that you can chew normally. The whole system becomes very unstable once the root wall is damaged.
Broken teeth or broken crowns can sometimes not be reattached.
The remnants of the root that remain in the oral cavity are often removed to avoid infection or to make space for an implant.
Read more on this topic at: Broken tooth - what to do
The root canal can also be treated if it does not have a longitudinal fracture. The remaining nerve residue is removed together with the blood vessels and the invading bacteria and an antibacterial filling material is introduced into the cleaned canal instead. The root residue treated in this way can now be used as an anchorage for a crown with a post.
A post is cemented into the root and a custom-made crown is placed on this post. This cannot always be done in this way.
The dentist must decide on the spot whether this treatment is an option or not. Decisive factors are, among other things, X-ray image, fracture location and periodontal conditions.
Crowns and a root canal treatment are very expensive and the costs for them are rarely fully covered by both statutory and private health insurances.
Not every patient is able to pay for the required crown or root canal treatment.
In this case, the dentist will remove the tooth in question.
If you simply leave the tooth in the oral cavity, inflammation develops and the resulting pus leads to blood poisoning.
If a tooth has become so infected that very severe apical periodontitis has developed, which cannot be eliminated even with root canal treatment, tooth extraction is considered. Apical periodontitis is an inflammation of the tooth root at the tip of the root. A large amount of pus usually forms, which then puts pressure on the tooth nerve, causing massive pain. If the inflammation is still in the early stages, an attempt is made to eliminate the focus of inflammation with a root canal treatment.
Read more on the topic: Root canal treatment
If the periodontitis has spread too far, an attempt is sometimes made to save the tooth by means of a root resection.
An oral surgeon removes a small bone window above the diseased tooth and cuts the inflamed root tip.
Sometimes the chances of success are small compared to the risk of the operation.
Patients with heart problems often cannot be adequately anesthetized or wound healing is impaired in some. In these cases, tooth extraction is more useful than surgery.
The weighing of the risks against the probability of success of the operation decides on further therapy. If the decision to resect the apex is not made, this will be carried out by the oral surgeon in a specially equipped practice.
In some patients, especially children, it is found that the jaw is too small for all 16 teeth.
In this case, the orthodontist orders the strategic removal of one tooth to make room for all of the other teeth.
If that doesn't happen, the teeth slide over each other in the jaw and the result is crooked and crooked teeth.
Of course, tooth extraction is also the last resort in this case.
The orthodontist must first make sure that even with braces you cannot create enough space for all your teeth.
Only when this is established is a tooth removed and the brace used to move the remaining teeth to the right place.
In the context of orthodontic treatment, the term "Equalization extraction". This means that a tooth is also removed from the opposite row of teeth to ensure that the patient can bite properly.
The occlusion is restored.
This is necessary, for example, if a tooth has not been created somewhere or had to be extracted to make room or if it would shift the center line between the incisors from the center of the face.
Carrying out the tooth extraction
In a normal dental practice, only teeth that have already erupted are removed! So only teeth that can already be seen in the oral cavity.
Shortly before the extraction, the tooth and the surrounding mucous membrane are anesthetized (pain elimination).
A conduction anesthesia is placed in the lower jaw and an infiltration anesthesia in the upper jaw.
Depending on the anesthetic, the effect will decrease approx. 3-10 min a.
Read more on the topic: Dental pain elimination
To extract a tooth, the first step is to use a chisel to stretch the alveolus. Without prior loosening, a dentist needs a lot more strength to tear the tooth out of its anchorage! The chisel actually has a certain similarity to the one from the hardware store, only it is much more filigree and finer. The alveolus is the bone compartment in which the tooth is firmly anchored.
Only when all the tendons and fibers that hold the tooth in the bone are loosened, special pliers are used to finally remove the tooth from the oral cavity.
There are different types of pliers. For example:
- the anterior forceps,
- the premolar forceps,
- the molar forceps,
- Root forceps,
- Whitening forceps.
So each tooth holds its own special forceps. At the same time, a distinction is also made between whether the tooth is to be extracted in the upper or lower jaw. The appropriate forceps are applied to the loosened tooth and an attempt is then made to remove the tooth. For single-root teeth (Front teeth and premolars) an attempt is made to turn the tooth.
Due to the anatomical position of the holding fibers, the forces that simply pull upwards offer great resistance, but they can hardly counteract rotating forces. Multi-rooted teeth (Molars or molars) cannot be rotated. The more periodontal damage the tooth was, the easier it is and the less force it can be removed.
In the now empty alveolus, a blood clot forms as a natural wound closure. A sterile swab is pressed onto the empty alveolus for about ten minutes until coagulum forms.
In most cases, the wound does not need to be sutured and the swab is absolutely sufficient.
Sutures may be placed in the case of very heavy bleeding or patients taking blood thinners.
Patients who take very strong blood thinners and who consequently have extremely heavy bleeding are sometimes given individually adjusted bandage plates in advance, which they are not allowed to remove until the check-up a day later.
Pain during and after tooth extraction
Pain while pulling
Before the tooth extraction, the affected region is anesthetized and a few minutes are waited for the local anesthesia to work optimally. During the extraction, the patient does not feel any pain, but he does feel a feeling of pressure, which comes about when the dentist uses a lever and exerts force. This feeling can be very uncomfortable, but is of the quality, if at all only a slight pain.
If an extraction takes longer, so that the effect of local anesthesia wears off, it can be re-anesthetized without any problems. A combination of several anesthetic techniques also accelerates the sound of the syringe. Nevertheless, there are cases in which the anesthesia does not work well or hardly at all, so that the patient feels pain during the procedure. This is the case, for example, with severe inflammation. If the tissue around the affected tooth is severely inflamed, the pH value is shifted to the acidic range, which is why local anesthesia does not work there.
Furthermore, the patient can be a so-called non-responder, which means that the anesthesia generally does not work. Drug users are also likely to experience pain on extraction through an inoperative syringe. In addition to drugs, alcohol consumption on the day before the extraction also has the effect that local anesthesia does not work. A glass of wine in the evening can mean that the syringe does not work the next day.
You can find more information here: Local anesthesia at the dentist
Pain after pulling
Pain after an extraction is not the norm. The removal of a tooth is a routine procedure that is usually associated with pain-free and uncomplicated wound healing. Complaints after extractions occur primarily during longer interventions that turn out to be more complicated and for which more effort is required. The force exerted by the dentist when pulling with the forceps or when using the lever irritates the surrounding tissue and the support on the neighboring teeth can cause discomfort in the first few days after the procedure.
There is a slight pressure pain and chewing on the affected side appears uncomfortable. However, these complaints disappear completely after a week at the latest. Wound pain is also possible because the alveolus has to close again. Pain occurs when bacteria infect the wound and inflammation develops. The patient feels the typical signs of inflammation with pain, possible swelling, reddening and noticeable warming.
The wound closure is prolonged by the inflammation. If, after the tooth extraction, the blood, which is converted into connective tissue cells in the tooth socket, is flushed out, the phenomenon of the empty alveolus occurs.
Read more on the topic: Wound healing disorder on the tooth
The germs now have direct access to the bare bone via the tooth socket and can infect it. The medic speaks of one Alveolitis sicca. The alveolitis causes severe pain due to the infection, in which the patient must necessarily go to the treating dentist. If alveolitis sicca is left untreated, pus may develop and develop into one abscess collects. This leads to severe swelling of the cheek, pain and even difficulty swallowing and breathing.
You might also be interested in this article: Toothache - what to do?
What can you do about the pain?
The patient should keep as calm as possible after a tooth extraction and not do any strenuous work. In addition to resting, targeted cooling helps against wound pain and prevents swelling and inflammation from spreading. If the pain is still unbearable, pain medication is indicated.
The pain reliever of choice is ibuprofen because of its anti-inflammatory and analgesic effects. Paracetamol or Novalgin® should be used in the event of an allergy; any medication with the active ingredient acetylsalicylic acid is contraindicated due to the increased tendency to bleed, as it can trigger secondary bleeding. If the pain medication still does not help, the dentist should be visited for follow-up care, who may prescribe stronger medication such as opiates.
You may also be interested in this article: Painkillers for toothache
When do you have to take antibiotics?
There are two ways in which an antibiotic is used when a tooth is extracted. Either it is used preoperatively, before the procedure, as a single dose to prevent infections. Most interventions do not require this prophylaxis, however, as tooth extraction is a routine procedure. Only in the event of complications during or after the procedure will the dentist initiate antibiotic therapy in which one tablet is taken two or three times a day for 5 days.
This antibiotic therapy can be used for severe inflammation Alveolitis sicca or an abscess that has formed. The practitioner decides in each individual case which preparation is prescribed in which dosage. The classic antibiotic is that Aminopenicillin amoxicillin. It is necessary to take the antibiotic for a long time so that no resistance develops.
Complications / risks
As with any procedure, complications can arise when extracting a tooth. In addition, as with any procedure, there is some risk.
The likelihood of serious complications is negligible!
For example, the root of the tooth can fracture and then has to be laboriously removed piece by piece.
If not all parts are caught, a cyst can still form around this part even years later, which must then be surgically opened and treated.
Also, such retained parts can be completely harmless and never develop symptoms.
After tooth extraction, wound healing disorders can also occur if the wound cannot be adequately closed by a "blood clot", as would be the case with healthy wound healing.
The wound healing disorder can have various causes, such as poor oral hygiene or smoking.
Read more on the topic: Wound healing disorder on the tooth
If the blood clot that has formed breaks down too quickly, the jawbone becomes inflamed because it lacks a protective layer and is completely exposed to the bacteria in the oral cavity.
Hard food, for example, can destroy the blood clot. This clinical picture is called dry alveoli or alveolitis sicca.
Opening the mouth can be difficult if a nerve was badly caught during the conduction anesthesia in the lower jaw. Most of the time, this will happen by itself after two to three days.
There is also a risk of hematoma formation due to bleeding into the surrounding tissue.
This hematoma is often accompanied by unsightly swelling on the face. Although this does not look very aesthetic, it is only dangerous or requires treatment in very few cases.
Pain is completely normal in moderation, only if pain persists for days or if there is no improvement at all, a dentist should be visited again.
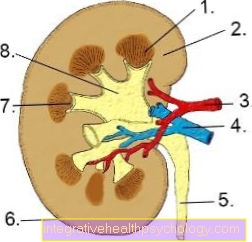
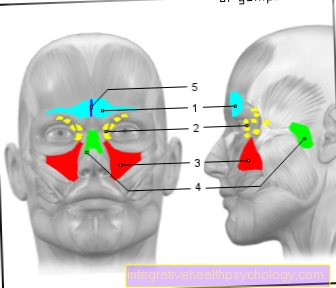
If a molar in the upper jaw (Molar tooth in the upper jaw) removed, it can happen that the maxillary sinus is opened.
The wall between the tip of the root and the maxillary sinus is very thin and can therefore easily break, which is not a fault on the part of the dentist.
After the extraction, it must therefore be checked whether an opening has taken place. If this is the case, this opening has to be closed again by the oral surgeon, because otherwise bacteria and germs from the oral cavity can get into the maxillary sinus and cause maxillary sinusitis there.
Opening the maxillary sinus is always an exception!
After tooth extractions, there are a few things that should be followed to ensure rapid wound healing.
Read more on the topic: Pull molar tooth
Pus after tooth extraction
Pus is always a sign of infection because it is made up of dead white blood cells.If pus forms, it is important to let this drain through a relief incision so that the pus collection does not enlarge and develop into a manifest abscess. In the case of already formed abscesses with severe swelling, a drainage system is made in addition to an incision to the drain, which consists of tubes through which the pus can constantly drain. Additional antibiotic therapy is also ordered to get the bacteria out of the body as quickly as possible and to prevent them from entering the bloodstream as sepsis. It may be the case that the patient is called in closely at the beginning of the day to completely drain the pus and to rinse the infected wound.
This article may also be of interest to you: Inflammation of the gums with pus
Bleeding after tooth extraction
Secondary bleeding is usually the result of incorrect behavior after an extraction. The active ingredient acetylsalicylic acid in many painkillers is the most common cause of self-produced bleeding due to its blood-thinning effect. Therefore, the attending dentist always explicitly advises not to take pain relievers such as Aspirin® or Tomapirin®. Furthermore, the consumption of alcohol after the procedure can thin the blood in such a way that secondary bleeding occurs. If secondary bleeding is detected, the patient should roll a handkerchief and bite it with pressure for ten minutes to stop the bleeding. If this does not stop the bleeding, the dentist or emergency service must be consulted immediately, who will close the wound with a flap and a close-meshed suture so that the bleeding is stopped.
Bad breath after tooth extraction
Bad breath after tooth extraction is in the majority of cases a sign of infection. Dead white blood cells form pus, which causes an unpleasant odor in the oral cavity. This smell only disappears again when all the pus has been drained and the inflammatory cells disappear. Furthermore, an unpleasant odor can arise from food residues that remain in the wound and cannot be cleaned. This creates a putrefactive odor that can be reduced by using rinsing solutions and cleaning wounds. Also one Alveolitis siccain which the blood is removed from the tooth socket, can produce unpleasant smells and bad taste. The smell only disappears when the wound closes and the inflammation subsides.
You might also be interested in this article: How to successfully combat bad breath
Is tooth extraction possible during pregnancy?
Dental interventions should generally be avoided during pregnancy and tooth extractions are only performed in extreme emergencies. Care must be taken to ensure that a local anesthetic with a high protein binding rate is used so that as little of it as possible can reach the unborn child. Since the procedure is always associated with stress for mother and child, it should be considered beforehand whether a Trepanation, the removal of the nerve tissue of the tooth is insufficient to relieve the pain and the tooth extraction is connected after the birth.
You may also be interested in this article: Toothache During Pregnancy
Is a tooth extraction possible despite Marcumar®?
Patients with heart disease are often stopped by long-term therapy with anticoagulants such as Marcumar®. Marcumar® thins the blood, which causes bleeding during tooth extraction that can hardly be stopped. Therefore, in consultation with the family doctor or internist, the drug is discontinued for the procedure and the patient is bridged with a replacement preparation, usually heparin. On the morning of the procedure, the value of Marcumar® in the blood is checked, the so-called Quick value. Tooth extraction is possible from a Quick value> 35%, if the value is not reached, the patient waits until the blood is "thicker" again. On the day after the procedure or on the day itself, Marcumar® is taken again, which is why a tight suture of the wound edges is essential to avoid rebleeding.
Behavior after the procedure
Immediately after the procedure, the area can be cooled for a swelling to avoid. Often patients complain of one swollen cheek.
Hard food should only be consumed after about a day in order not to tear open the wound again and again.
Contain dairy products Lactic acid bacteria, which can prematurely dissolve and destroy the blood clot. There is a risk of those already discussed Alveolitis sicca.
The dentist usually gives you a prescription or tablets to take home with you against any pain that may arise.
Is common Ibuprofen the means of choice.
Any pain reliever can be used not at the same time as a blood thinner works.
The day before and one to two days after the extraction should not be aspirin be taken because it thins the blood and greatly affects wound healing.
Also caffeine has a blood-thinning effect and should therefore only be consumed in moderation one to two days after the procedure.
On Smoke should also be avoided until the wound has healed, as the smoke extremely slows healing.
The extraction wound will heal after about a week.
When can I eat again after the procedure?
Eating after a tooth extraction is possible when the anesthesia has completely subsided. Before that, the risk of injury is too great as the cheek parts, tongue and lip can be numb and the patient does not notice if he bites the affected area or if the tea or soup is too hot. After the local anesthesia has expired, soft foods should be used for the first few days, hard foods such as nuts should be avoided in order not to overload the teeth in the affected area. Coffee should also be avoided as it increases blood pressure and blood flow, which can lead to inflammation.
What role does homeopathy play after tooth extraction?
Homeopathic aids can support dental therapy, promote wound healing and strengthen the weakened immune system to prevent infections. Nevertheless, it is important to discuss the intake with the treating dentist in order to find the right preparation. After tooth extractions, granules of choice are arnica and calendula in D12, which can relieve swelling and pain. Bellis perennis and Chamomilla recutita In the D12 potency, infections can be counteracted and symptoms contained. The globules are effective against pain after the treatment Belladonna, also in D12. The correct dosage of all these globules is three times a day for five globules.
Further information can be found here: Homeopathy for toothache
When can I start smoking again after the procedure?
Smoking is contraindicated after tooth extraction, as it disrupts the healing process and promotes infection. The contained carbon monoxide and nicotine reduce the oxygen content, which is essential for wound healing. Furthermore, the blood circulation is worsened by smoking immediately after the procedure. The tar from the cigarette can be deposited in the wound and prevent the blood clot from converting into connective tissue cells within the wound. The process of wound healing is slowed down, and severe pain can also arise due to infections. The bacteria have easier entry into the wound after extraction and, in the worst case, can cause blood poisoning, known as sepsis, with life-threatening consequences. Therefore, smoking should be avoided for the first three days after tooth extraction.
When can I drink alcohol again after the tooth extraction?
Alcohol after tooth extraction is contraindicated as it has a blood thinning effect and disrupts clotting. If the patient drinks alcohol after the procedure, there is a risk of secondary bleeding, which will result in a visit to the dental practice for subsequent treatment. Furthermore, alcohol also increases the risk of infection. The bacteria can settle in the wound more easily and multiply faster because the blood flow is increased. It is therefore necessary to abstain from alcohol for at least three days until the wound edges have approached and almost closed.
Duration of healing
The duration of healing goes hand in hand with the removal of the stitches. Sutures that have been set should be removed after seven to ten days, by which time the wound has grown closed in the majority of cases. The wound is closed, but the gums are not yet completely leveled. The bone in the tooth socket also forms, which can take about four to six weeks, but the patient hardly notices this process.
If there are complications, however, the phase can continue until the wound closes, so that after seven to ten days after the sutures are pulled, the wound edges are not yet closed. If the infection persists, the dentist can clean and scrape out the socket again, so that a new clot of blood is created, which is converted into connective tissue.
In the case of complications, it is not possible to say in general how long the healing will take, because other factors also play a role. Smokers and patients with diabetes mellitus have impaired wound healing, which favors infections and in principle already prolongs the closing of the wound edges. In general, it is important for the patient to go to the dentist for a follow-up check after the tooth extraction, even if there was no suturing, in order to have the wound healing checked. If symptoms arise, the patient should visit the dentist immediately to initiate the necessary measures.
How long will I be on sick leave?
In the case of uncomplicated interventions, no sick leave or only one sick leave for the day of treatment is usually necessary. If complications arise in wound healing, the dentist can issue a one-week sick note, depending on how quickly the situation stabilizes. A daily follow-up check is the rule.



.jpg)