Wound healing disorder
General
A wound healing disorder is generally understood to mean the slowed, untypical process in the natural healing of a wound.
There are a variety of reasons a person can develop a wound healing disorder:
Individual characteristics or illnesses as well as external factors, such as the incorrect care of a wound, can lead to wound healing disorders.

causes

Healing a wound is a complex process. In order for a wound to heal at normal speed and correctly, various processes in the body must run correctly and interlink: a large number of different cells and signal substances and a supply of sufficient nutrients via the blood are necessary so that the injured tissue is finally replaced and the wound can be locked. As soon as any part of this system is disturbed, a wound healing disorder can arise.
Read more on the topic: Superinfection
In principle have elderly a higher risk of wound healing disorder than younger people. This is because in old age the Blood circulation the skin decreases and the performance of the Immune system is less. A weakened immune system is also generally, regardless of whether it is due to certain diseases (tumors or chronic infectious diseases such as tuberculosis or HIV) or medication (Cortisone) always promotes the development of a wound healing disorder. In addition to the drugs that affect the immune system, there are also drugs that have a direct negative effect on the ability of wounds to heal. These include anticoagulants (for example Heparin) or cytostatics (various Chemotherapy drugs).
There are many diseases that make a wound healing disorder more likely: Anemia (anemia), peripheral circulatory disorders (PAOD), Diabetes mellitus, venous insufficiency (Varicose veins). Almost all of these do this mainly by leading to a poor oxygen supply in the tissue, which slows down wound healing. The same mechanism affects the consumption of nicotine (when smoking cigarettes) has a negative effect on wound healing.
Another common reason for wound healing disorders is poor nutritional status. At a Malnutrition, so when it comes to the body Carbohydrates, Fats, Proteins, Trace elements, Minerals or Vitamins If it is missing, the damaged tissue cannot be adequately supplied with nutrients. (Please also read: Zinc deficiency) Are particularly important for wound healing Calcium and vitamin C. In general, both too little (because of the resulting deficiencies) and too much (because of the resulting excess weight) intake of calories are bad for the process of wound healing.
In addition, there are certain properties of the wound itself that predispose to wound healing disorder. These include large, soiled and bruised wounds, bruises or other accumulations of fluid (seromas) in the area of the wound, failure to immobilize the wound or removing the sutures from a surgically created wound too early, tension (when the surgeon sutures with too much tension has) or a divergence of the wound edges.
Symptoms
The symptom of the wound healing disorder is ultimately the non-healing wound itself. Depending on the type of wound healing disorder, the edges of the wound may diverge (wound dehiscence), enclose an accumulation of blood (wound hematoma) or be dead and thus yellowish (wound edge necrosis). As a result of inflammation processes, the wound and sometimes its surroundings can be reddened or, less often, swollen, cause itching or even pain. Some wounds are also oozing. If certain germs enter an open wound, further serious symptoms can develop that are no longer localized, for example fever.
Another and much rarer form of wound healing disorder is the so-called keloid. For unknown reasons, excessive scarring occurs here. The wound grows closed due to the overproduction of connective tissue, but the resulting scar is extremely large and raised.
Laser therapy is best for treating such scars. Read more about this under: Laser scars
diagnosis
A doctor can usually diagnose a wound healing disorder as Eye diagnosis be asked. It is more difficult to find out the cause (s) of the wound healing disorder. To do this, the doctor first asks his patient exactly what caused the wound, how long it has existed and whether it has changed over time. This medical history survey (anamnese) one closes examination the wound. The doctor takes a close look at the wound and how far it has healed (or not). If a causal factor is suspected Underlying disease Further examinations may be useful, which then serve to diagnose this specific disease.
therapy

There are many different methods that can be used to treat a wound healing disorder. Which of these is ultimately selected depends primarily on the Status the wound, the patient as an overall picture (underlying diseases must always be included in the therapy planning!) and also on the patient's ideas.
First of all, it is always important to thoroughly clean the wound clean. This is preferably done with a so-called Irrigation solution, which is usually either Saline solution or one with Calcium and potassium ions enriched Ringer's solution. The rinsing is carried out to avoid any Germs and foreign body, Cell debris and remove dead tissue from the wound. In the case of germ-laden wounds, a antiseptic rinse solution can be used. If the irrigation does not give a sufficient result, the dead tissue can alternatively operational removed. The wound is then sutured (again). Such a "Debridement“Should only be done if a good blood supply to the tissue can be assumed. Because wounds generally heal better when they are in a humid and warm environment nowadays, wounds are usually covered relatively generously with soaked compresses. Alternatively, you can use special gels and foams. It is important that the bandage is changed regularly, but not too often, as this could interrupt the healing process. In order to further support this healing process, certain substances can be applied (for example Hyaluronic acid) or taken (Vitamins, anticoagulant drugs) become.
In the context of the therapy of a wound healing disorder, it is also of great importance to discover an underlying disease and also to treat it, otherwise the wound cannot heal properly despite the above measures.
Contractubex against wound healing disorders
Contractubex® can be used for various forms of scars that arise in the context of wound healing disorders.
Atrophic scars (i.e. not enough connective tissue is formed) or hypertrophic scars (in which too much connective tissue is formed) can develop in wound healing disorders.
The early application of Contractubex®, immediately after wound closure, can counteract such complications of wound healing disorders.
It is available as a gel to massage in or as an intensive patch to stick on overnight.
You can find more information on the topic here: Contractubex®
course
When wound healing disorders early recognized and timely receive adequate therapy, they are not another cause of great concern. Especially with very large wounds, such as those caused by operative interventions arise, but it can become massive in the case of inadequate or unsuccessful therapy Inflammation and thereby lead to life-threatening conditions. Therefore, one should consider people who can be assumed to have a tendency to impaired wound healing (for example the elderly with diabetes), always carefully consider whether an operation is actually necessary and, if so, check the patient and his wound closely afterwards.
Phases of wound healing
The Wound healing can generally be in three phases be divided, whereby these do not have to follow one another strictly, but rather blur into one another or can even run partially parallel to one another.
- The first phase is the so-called Cleaning phase (also exudative phase), which occurred in the time from the immediate injury to approx 3rd day of wound healing lasts. In this phase the Hemostasis and Blood clotting instead, which then changes into an increased secretion of blood plasma into the intercellular tissue through subsequent vasodilation and increase in vascular permeability. This will make that Immigration of immune cells into the wound area, so that this subsequently break down broken cell material and a antibacterial environment can create.
- The second phase is the Granulation phase, which starts on the 4th day and continues until about 5th / 6th Day persists. In this phase it comes to Cell and blood vessel formationso that the primary wound defect is covered by a first so-called granulation tissue.
- The last to follow is the Differentiation phasethat are predominantly between the 6th and 10th day of wound healing takes place. The granulation tissue gradually matures and slowly closes scar tissue with less water and less blood vessels, Collagen fibers are incorporated, the wound contracts and new epithelial cells migrate in. Whether a wound is remodeled with scarring or completely regenerated depends largely on the depth of the wound.
prophylaxis
There are several measures that can be used to counteract the development of a wound healing disorder. Certain factors, such as age or certain illnesses, cannot of course be influenced, which means that certain groups of people simply have a higher risk of impaired wound healing than others. However, it is still possible to reduce the likelihood of this disease. This can be achieved above all by always paying attention to the correct treatment of an existing wound. For the patient, this means keeping the wound clean, moist and calm and for the surgeon to ensure that the wound edges are tensioned appropriately.
Read more on the topic: Phases of wound healing
In addition, risk factors such as malnutrition or obesity should be reduced. In addition, one should of course make sure to strengthen the immune system and ensure a balanced diet. If certain underlying diseases are present, it is important to treat them appropriately in order to prevent the development of wound healing disorders. In addition, it is of course absolutely necessary to consult a doctor as soon as possible if a wound healing disorder is suspected (i.e. as soon as a wound does not heal as easily as usual) so that he can initiate adequate treatment.
Even with stab wounds, there is a risk of infection. For this reason, the stab wound should be kept as clean as possible. Read more about it below: Stab wound
Wound healing disorder in smokers
The Absorption of cigarette smoke and the contained therein, harmful ingredients, proven to affect the Wound healing negative, so that numerous studies could show that smokers have a significantly delayed and poorer wound healing than non-smokers.
The cause lies in several harmful influences from the nicotine:
For one regulated, uncomplicated wound healing is the unrestricted functioning of certain cell lines in the body such as B. the Fibroblasts (Cells that are responsible for the formation of new connective tissue) and Macrophages (Immune defense cells). These have to multiply sufficiently in the wound area and form and release the growth factors necessary for healing.
The one in cigarette smoke nicotine on the one hand bothers them Mobility of the fibroblasts, which thereby preferentially stick to the wound edges and one slower wound closure as well as a increased scarring cause. On the other hand, nicotine stimulates the formation and The release of growth factors is restricted.
Furthermore, the nicotine leads to the fact that in the body of the smoker the Narrow vessels, which is particularly strong in the vessels of Hands and Feet makes noticeable. On top of that, smokers in general less good with oxygen in the blood are supplied, as non-smokers, since the carbon monoxide absorbed with the cigarette smoke occupies the binding sites for the oxygen molecules on the red blood cells.
In addition, nicotine amplifies the Release of stress hormones like adrenaline, which further increases the oxygen consumption in the body.
The generally reduced oxygen supply and the deteriorated blood circulation - especially the terminal areas on the hands and feet - therefore leads to one Undersupply of the wound areas with oxygen and nutrients, so that healing can no longer proceed optimally.
Wound healing disorder in the area of the tooth
Fortunately, wound healing disorder is in the area of the Tooth relatively rare. Most often the disease can be resolved after a Operation on the dentition like one Tooth extraction (lat .: extraction) observe. Usually our body can do one in a short period of time stable blood clot (lat .: Coagulum) and so the Close the defect. Immigrating cells and small blood vessels ultimately turn the wound into scar tissue. After a while, there is no longer any difference to the surrounding region.
With a wound healing disorder, however a stable coagulum does not arise for various reasons. Destroyed tissue cannot be broken down properly and forms an excellent breeding ground for Germs and bacteria. infection and inflammation cause painful wound healing disorders.
Especially large and deep wounds in the lower jaw are particularly affected (e.g. after removal of wisdom teeth). In addition to the size of the wound, behavior and habits after the dental procedure also play a role. So especially suffer Smoker significantly more often with a wound healing disorder in the area of the tooth. Also alcohol, acidic drinks and physical activity immediately after the procedure increase the risk.
In order to prevent wound healing disorders, those affected can take a few simple measures to heart. So, despite the wound, you should practice careful oral hygiene with a soft toothbrush. Just leave out the injured area! Disinfecting mouthwashes (e.g. with Chlorhexidine) also prevent bacterial growth.
With especially large wounds or other risk factors, such as a poor defense, your dentist will already arrange one antibiotic prophylaxis for the prevention of wound healing disorders.
If the measures described are unsuccessful, patients may suffer 3 days after tooth extraction severe, throbbing pain in the operated area. Often, they shine Pain in the face (temple, eye etc.). In severe cases a general feeling of illness can be observed fever, Slackness and a headache observe. Timely treatment is hugely important now! Your dentist will first try to deal with the infection Antibiotics to manage. The last option is another one surgical intervention in question.
Wound healing disorder after an operation
After an operation, many patients are initially relieved when everything has gone according to plan. Unfortunately, many complications can still arise after the operation has been overcome. One of the most important and feared complications is wound healing disorders. It delays wound healing in some cases considerably and can lead to significantly longer inpatient hospital stays.
The causes are very different. On the one hand, they depend on individual factors, such as Age, previous illnesses and obesity. On the other hand, of course, the operating conditions play a role: the operating area, size of the wound, suturing technique and hygiene are only to be mentioned here as examples.
In spite of state-of-the-art medicine, wound infections can often be observed, especially in hospitals. They are among the most dangerous wound healing disorders after an operation and in some cases even end in death. At the beginning, the infection of the wound is noticeable by a slight reddening and / or swelling. In the course of the disease, many patients report pain and pus leakage. Now it is important to take therapeutic measures (e.g. vacuum bandages, wound cleaning, etc.) in good time, as otherwise the infection can spread to other parts of the body. In many cases, antibiotic therapy is suitable for this. Wound swabs may be performed to be absolutely sure. With this method, the smallest amounts of wound secretion are removed and analyzed under the microscope. This can be used to determine which bacteria are causing the infection. A targeted antibiotic therapy can then be planned. Infections with multi-resistant germs (MRSA) in particular are currently posing real challenges for many clinics.
Since wound healing disorders z. Sometimes it can go very quickly, it is very important after the operation that the treating physicians carry out regular wound checks. It is essential to look carefully under the bandage and not just examine the surrounding tissue.
This article might also interest you: What is a hernia?
Disorders of wound healing in diabetes
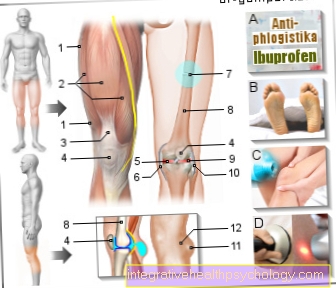
Diabetes is one of the most common causes of wound healing disorders in Germany. Patients often suffer from protracted, weeping wounds and in some cases are significantly restricted in their quality of life. But why is that? As a complex disease, diabetes intervenes in various processes in our body. Long-term elevated blood sugar levels damage our small and large blood vessels. The doctor then speaks of a "micro- or macroangiopathy". Crucial for the development of a wound healing disorder are mainly Damage to small blood vessels. Because their progressive destruction leads to a reduced blood flow in affected body regions. At the beginning, this mainly affects the feet of the diabetic patient and later the legs. In the course of time, however, a wound healing disorder can also be observed in all other parts of the body. The diabetic foot is also popularly known. This leads to a chronic wound healing disorder in the area of the feet, which in the worst case culminates in an amputation. Diabetes patients should therefore have their feet checked by a doctor at regular intervals.
In addition to the damage in the blood vessels described, diabetes also damages the nervous system. With this disorder, there is permanent damage to the sensitive nerves. Patients report abnormal sensations (“burning feet”), numbness, “pins and needles”, and disturbed temperature and vibration sensations. As part of this “diabetic polyneuropathy” (PNP), those affected simply no longer feel small injuries. Especially on the feet, originally small wounds can trigger serious wound healing disorders with infection. For prevention, diabetics can e.g. fall back on specially padded shoes or made insoles.
Furthermore, diabetics often have a weakened immune system. Due to the reduced defense, germs can settle more easily and sometimes trigger dangerous infections.
Basically, the blood sugar of a diabetes patient must be adjusted as optimally as possible. This is the only way to prevent permanent wound healing disorders and serious consequences.