Chest pain while breastfeeding
Definition - What is Breast Pain While Breastfeeding?
There are several causes of breast sore while breastfeeding. A distinction should be made between pain that only occurs during breastfeeding itself and pain that is permanent and is also expressed during breastfeeding. It is important, however, that in most cases you can do a lot with heat and massage of the breast. However, if there is bacterial inflammation of the breast tissue, massage should not be used, as the germs can then be distributed throughout the breast.

Causes of Chest Pain While Breastfeeding
In addition to the numerous causes of breastfeeding pain, there are four aspects that are highly relevant when looking for a trigger.
-
Painful initial milk penetration: This problem shows up after approx. 3-4 days and is mostly on both sides. There is a feeling of tension, enlargement, firm glands and a high sensitivity of the breast with vein markings. Frequent donning is very important. In addition, moist warmth or a massage from the inside out can also help beforehand. Emptying the chest by hand can also help. After putting it on, cold rather than warmth helps. Painkillers can also be used if necessary.
-
Sore nipple: 95% of the time a sore nipple is an unfavorable posture and therefore incorrect sucking behavior by the child. This can be caused by artificial teats or a shortened frenulum of the child's tongue, which makes it difficult to suckle properly. Other causes include a fungal colonization of the nipple (thrush) or a bacterial infection. Proper breastfeeding is important for the mother. Changing breastfeeding position or rubbing breast milk on the nipple can also have a positive effect. If this does not help, you should think about suckling training for the child.
-
Milk congestion: Milk congestion is a stress-induced problem. Stress promotes the production of milk but inhibits its release. This is a very unfavorable constellation with the consequence of a milk congestion. Pressure from bras, rucksacks or slings can also have a negative effect. Traffic jams tend to be one-sided and are often associated with palpable lumps, reddening of the chest and fever. Quiet and frequent breastfeeding are very important in management. Also read: Milk congestion- What can you do?
-
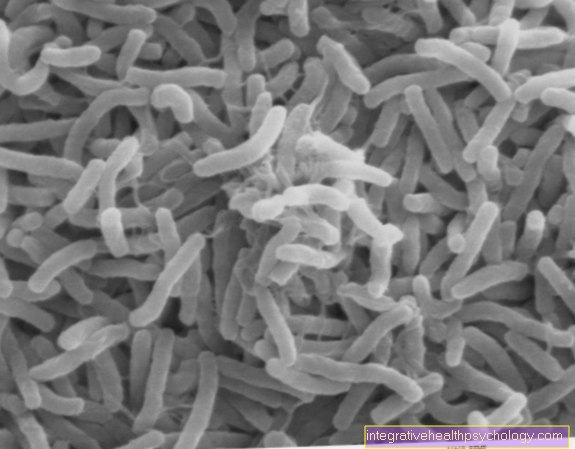
Breast inflammation (puerperal mastitis): Puerperal mastitis is an acute inflammation of the mammary gland in the puerperium. Usually within 2 - 4 weeks after birth, one-sided breast inflammation with pain, fever, flu-like symptoms and reddening occurs. The cause is usually the harmless skin germ Staphylococcus aureus. It is very important to note that you should continue breastfeeding despite this inflammation. Before breastfeeding, moist warmth and pain relievers will help. A massage is not recommended here. If you have a fever for more than 1 day you should start antibiotic therapy. The only case in which one should pause breastfeeding arises when both breasts are infected by so-called B streptococci.
Read more on the subject at: Problems during breastfeeding in the mother
diagnosis
If you have breast pain while breastfeeding, you should see a gynecologist to find the right diagnosis and to discuss how to proceed. In addition to a medical consultation and a palpation examination of the breast and lymph nodes, other diagnostic measures such as a blood test, ultrasound or a smear can also be helpful. This makes it relatively easy to detect an infection from various germs in the blood and smear. Ultrasound shows masses like an abscess. This is a newly formed cavity that is filled with pus. In order to rule out a malignant disease of the breast in the context of inflammatory breast cancer, a mammogram can also be performed.
Milk congestion
As the name suggests, milk congestion leads to a build-up of breast milk. An important factor for the development is stress. Regardless of whether it is due to too many visitors, an argument or too many well-intentioned tips from friends and family, care should be taken to eliminate all stress factors. However, a nursing bra that is too tight or a lack of sleep can also lead to this.
Milk congestion usually presents with pain, redness, swelling, fever, and chills. However, it is important to empty the breast regularly about every 2 hours despite the pain. A massage of the breast and lots of heat as well as stroking the mammary glands help to promote the flow. Many women find expressing more comfortable than sucking the child, as the breast is completely emptied.
Once the traffic jam has been cleared, the pain usually becomes significantly better. However, it may take a few more days for all symptoms to resolve completely. Quark compresses or cool packs can be used to cool after breastfeeding. However, only heat should be used before breastfeeding.
For more information on treatment, see: Milk congestion- what can I do about it?
Inflammation of the breast (puerperal mastitis)
Inflammation of the breast (mastitis puerperalis) in the puerperium usually occurs about 2-4 weeks after delivery. In the vast majority of cases, the inflammation is caused by the skin germ Staphylococcus aureus. This bacterium is found on everyone's skin and does not cause any problems. Breastfeeding, however, leads to small tears in the sensitive skin of the nipple and thus offers the germs a portal of entry. Inflammation of the female breast occurs. The inflammation is usually limited to only one quadrant, which is noticeable by pain, redness, swelling of the breast and lymph nodes and overheating.
However, breastfeeding should definitely be continued so that there is no additional traffic jam. The milk does not have to be discarded either, as was previously taught. Antibiotics are also not necessary in most cases. If the fever lasts longer than a day, antibiotic therapy should be considered. If you suspect an abscess, i.e. an encapsulated area filled with pus, a gynecologist should be consulted.
These articles might also interest you: Can I breastfeed with a fever?
Concomitant symptoms
Chest pain is usually accompanied by accompanying symptoms. These can provide clues as to the underlying causes and show therapy options more clearly.
fever
Fever is a classic symptom of bacterial inflammation. In the context of a breast infection during breastfeeding (mastitis puerperalis), a fever can be an indication of this.
However, a fever can also occur if the milk is blocked. As a rule, milk congestion is less severe and lasts up to 2 days. However, the blocked milk can also become an infection with bacteria that colonize the breast and make the course more difficult.
Both symptoms can lead to fever and chills.
Redness of the chest
If the chest becomes red, this indicates irritation of the tissue and often inflammation. This can have different causes. A diagnosis that should be clarified is puerperal mastitis, an inflammation of the breast after birth. It arises from a mostly bacterial infection and can be treated well. But milk congestion can also be noticeable through reddening.
Another important diagnosis that should definitely be ruled out is inflammatory breast cancer. This is a breast cancer that looks like an inflammatory reaction but does not respond to typical therapies. Therefore, one should palpate both the breast and lymph nodes by a doctor in order not to miss this condition.
Stinging in the chest
Most people associate a stabbing sensation in the chest with a heart attack. However, it is also not uncommon in breastfeeding women and has nothing to do with the heart here. In the vast majority of cases, there was previously a fought inflammation, the aftermath of which can sometimes be painful.
Alternatively, there may be a chest thrush. This is a fungal disease caused by Candida albicans or its spores.In itself, the fungus is rather harmless, but can also cause problems when breastfeeding. The infant also carries the fungus in the mouth. There are several factors that can make such an infection more likely to break out. This includes everything that ensures a weakened immune system such as fatigue, stress or malnutrition. Diseases such as diabetes or various medications can also be responsible for this. Anyone who takes an antibiotic due to a bacterial infection must also expect that the destruction of the bacteria will create a perfect place for the fungus to spread.
also read: Oral thrush in babies
Body aches
This usually occurs during breastfeeding due to blocked milk or an inflammation of the breast, which is caused by bacteria. However, it can also occur independently of a breast disease as a sign of a cold or a flu-like infection.
a headache
Like many other symptoms, a headache can indicate a blockage of the milk which, due to bacterial overgrowth, can lead to inflammation of the breast during breastfeeding. Other causes of headaches can be iron deficiency or insufficient drinking. Since a large part of the fluid available to the body is used for the production of breast milk, this volume is missing elsewhere. Therefore you should pay attention to sufficient fluid intake. A drinking amount of 1-2 liters should therefore be observed. However, those who drink too much or too little can also have a negative impact on milk production.
node
If areas of the breast are nodularly changed during breastfeeding, a very harmless cause such as milk congestion may be behind it. When breastfeeding, the position of the child should therefore be changed more frequently during breastfeeding and also be oriented towards the hardening. Thus, an attempt can be made for the infant to suck off the milk from different areas of the breast and thereby remove the congestion.
However, if in doubt, a doctor should be consulted in order to be able to rule out breast cancer as a diagnosis.
Also read: What types of breast cancer are there?
Chest pain without hardening of the chest
A sore chest can be associated with or without hardening. A hardening is usually a blockage of the milk. However, an incipient milk congestion does not immediately manifest itself as a hardening and should be treated with moist warmth and a lot of breastfeeding so that the congestion cannot build up too long in the first place.
When should i go to the doctor?
If you experience breast discomfort after breastfeeding, this is not a cause for concern at first. Rest and adequate treatment with frequent application, warmth or cold and possibly massage of the breast is important.
However, if the symptoms do not improve after 1-2 days, a gynecologist should be consulted. The cause of the problem can be determined here on the basis of a physical examination and palpation, but also with smears and ultrasound. Depending on the cause, drugs can also be ordered.
Therapy of chest pain during breastfeeding
Depending on the cause, the therapy is always different. Therefore, a recommendation cannot be made in such a general way. However, it is important that in the vast majority of cases breastfeeding should continue. If in doubt, a doctor can assess the risk and decide when to stop breastfeeding. It makes sense to try different positions for breastfeeding so that the child has comfortable access to the breast and causes less pain. You can use aids such as pillows or towels to find the optimal position. When putting it on, make sure that the mother is lying or sitting and the child is facing the breast. Also, moist warmth in the form of compresses just before breastfeeding is often helpful. If there is no infection, massaging the chest can also improve symptoms. Some women squeeze some breast milk out of their breasts and rub it on the nipple.
For more tips on how to breastfeed, see: Breastfeeding- everything you need to know about breastfeeding tools
In most cases, medication can provide pain relief. If you are infected, you may need to use antibiotics while breastfeeding. Which medication can be taken can be found on the “Embryotox” page, among other things.
Also read on this topic: Medication while breastfeeding or ibuprofen while breastfeeding
When do i need an antibiotic?
If a bacterial infection is prevalent, antibiotics can be taken if the mother's symptoms do not improve after 12-24 hours. However, it is important to ensure that the drug can be taken during breastfeeding so that some of the antibiotic does not get into breast milk. The pack should be taken to the end, even if the symptoms have already improved significantly beforehand. This is because relief comes when not all of the bacteria have been killed. However, if some germs survive due to a treatment that is too short, resistance can develop and the antibiotic becomes ineffective.
Which home remedies can help?
Approaches differ depending on the cause of the pain. As a rule, however, you can usually achieve a lot with heat. It doesn't matter whether this is achieved with a warm shower, a red light lamp or a warm washcloth.
As long as there is no infection, a massage can also help. By using oil, the fingers slide better over the painful chest and make it easier to knead the chest.
You can also try expressing the breast or laying the baby on frequently to help clear a congestion. Pumping is often more comfortable as the breast becomes emptier than when the child is drinking.
Another possibility are poultices with quark or white cabbage, which are supposed to provide relief and have a beneficial effect due to their anti-inflammatory and pain-relieving properties.
Quark wrap instructions
For quark wraps you need natural quark and a cloth to which the quark is applied. The cloth is traditionally coated with a thick layer of quark and carefully placed on the chest. The sensitive nipple should be left out so that it does not soften and become even more vulnerable. The wraps are left on until they no longer have a cooling effect. The quark is then washed off or showered off.
If you don't want to wash the quark off your chest, you can alternatively cut kitchen paper into circles and adjust them to the breast size. Again, the middle should be left out for the nipple. A thick layer of quark is then applied between two cut kitchen towels. The kitchen paper and quark construction can now either be placed in the refrigerator or directly on the chest. If you want to prepare this type of wrapping, you should put a layer of cling film between the individual wraps to separate the wraps in the refrigerator. Regardless of whether you cut kitchen paper or use towels, it is best to apply the compress to a pumped or vacuumed breast.
homeopathy
In the case of a blocked milk, you can try different methods to reduce the amount of milk and thus to alleviate the pain so that the treatment is easier and the blockage does not become too big. The homeopathic Phytolacca can be used for this. But everyday remedies such as peppermint teas or sage teas and candies can also reduce the amount of milk. However, you should consult a midwife or a gynecologist beforehand so as not to accidentally wean yourself too much!
However, with inflammation of the chest, hepar sulph, chamomile, bryonia, belladonna and many more can also be used.
For some women, acupuncture also helps with their chest discomfort.
Also read: Homeopathy for breastfeeding problems
Duration
Depending on the cause and the start of the correct treatment, the duration may vary. A milk congestion can get better within hours and is usually completely gone a few days later. Inflammation can last a few days to weeks. However, an abscess increases the duration.
It should be kept in mind, however, that all breastfeeding problems tend to recur.
When should I wean?
In principle, there is only one case in which one should stop breastfeeding due to symptoms: If both breasts are infected with the bacterial strain beta streptococci, breastfeeding should be paused for the duration of the inflammation. Many women who wean early experience painful breastfeeding. You should therefore try to find the optimal breastfeeding position. In the beginning it takes a little while for breastfeeding to work, especially with the first child. This is perfectly normal and takes practice. Both from the child and the mother. If in doubt, you can get help from breastfeeding advice or a midwife.

























.jpg)