Fat embolism
What is a fat embolism?
The fat embolism is an embolic event of fatty material in the vascular system.
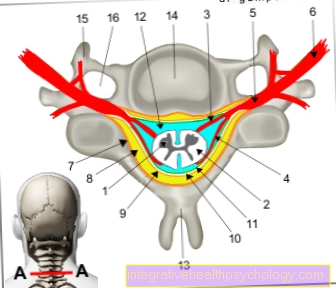
The occlusion can affect the pulmonary vasculature and, under certain circumstances, the vascular system of the central nervous system (CNS). This leads to serious complications that can be fatal without being recognized.
In addition to the fat embolism, there are other forms of embolism. In addition to the classic thrombosis, there is also the amniotic fluid embolism, air embolism or bone cement embolism. Like the other forms, the fat embolism appears in the vast majority of cases as a pulmonary embolism. The fatty material of the embolism can arise from a wide variety of organ systems in the human body through a wide variety of disease processes. Pathophysiologically, there is an occlusion of the small pulmonary vessels with a deterioration in gas exchange and the resulting stress on the right heart.

causes
Below you will find an overview of the most common causes of fat embolism. These are then explained in more detail.
- Broken bone
- Use of a hip prosthesis
- Liposuction
- Inflammation of the pancreas
Fat embolism after a fracture
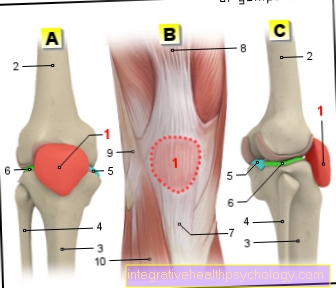
Fat embolism occurs primarily in closed fractures of long tubular bones.
These are mainly the humerus, thigh bones, shin bones and the fibula bones. Due to their elongated structure, these contain a relatively long marrow cavity, which is primarily filled with bone marrow containing fatty tissue. With a closed fracture of these predestined bones, part of this fatty bone marrow can detach itself into the vascular system.
- Femur fracture
- Upper arm fracture
Fat embolism after hip prosthesis
Fat embolism can develop postoperatively in the orthopedic and trauma surgery specialist area.
Here it can, for example with hip replacement (Total endoprosthetics) can lead to complications of fat embolism. By inserting the prosthesis shaft into the femur shaft, strong pressure is built up on it. By compressing the fatty bone marrow it contains, a fatty embolus can be detached. The heating of the bone cement material in the setting phase of the hip replacement can also lead to fat embolism.
Overall, the frequency of fat embolism in hip arthroplasty is between 1 and 10%. A fatal outcome occurs at 0.1 to 0.5%. An amputation increases the risk.
Further information on this:
- Complication of hip replacement surgery
- Post-operative complications
Fat embolism after liposuction
Even with liposuction (Liposuction) there may be an increased release of fatty material, with the formation of a fatty embolus.
However, the risk here is rather low. Typically, liposuction is more likely to lead to complications such as acute swelling and inflammation and, in the longer term, the development of skin dents and asymmetries.
You may also be interested in this topic: Breast augmentation with your own fatty tissue
Fat embolism due to inflammation of the pancreas
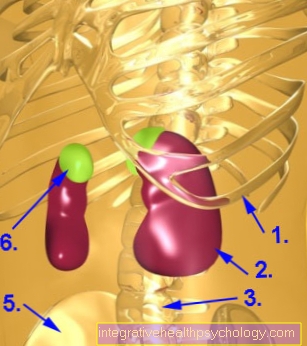
However, another cause of a fat embolism can also be one acute pancreatitis Alsoe be a pancreatitis.
The pancreas is an organ that releases certain enzymes used in the digestive process. Among them, especially for fat embolism, is the Lipase crucial. This enzyme plays a key role in breaking down the fats in the small intestine that are ingested through food. In acute pancreatitis, the lipase is accordingly released to an increased extent, which can result in a fat embolism.
More on this: Pancreatitis - How Dangerous Is It?
Symptoms
Typical symptoms of a fat embolism include:
- Difficulty breathing
- Petechiae
- Neurological symptoms and failures
- fever
- Heart rate increase
The first thing that typically occurs is difficult breathing, possibly even shortness of breath on. In addition, there is small skin bleeding (petechiae) on typical body regions, such as the head, conjunctiva, chest and armpit. The embolic occlusion of cerebral vessels can lead to neurological symptoms. These are mainly focal sensory disturbances and paralysis, decreased alertness and confusion.
Other symptoms include increased heart rate and fever. Accompanying anemia (anemia), a lack of platelets (Thrombocytopenia) and a high rate of blood sedimentation (ESR) occur. These are signs of an inflammatory process.
In addition, kidney failure with reduced urine production or changes in the fundus are possible.
You might also be interested in these topics:
- When abdominal pain and back pain occur together
- Acute respiratory failure
diagnosis
The fat embolism shows a noticeable clinical appearance, which should prompt the treating physician to suspect a pulmonary embolism. Pathological vital signs are clinically evident. The combination of a drop in blood pressure, an increase in heart rate and shortness of breath with a resulting increase in the breathing rate are typical of pulmonary embolism. The increase in pressure in the pulmonary vessels can put stress on the right heart. This is shown e.g. a so-called upper inflow congestion (congestion of the neck veins). A split second heart sound can also be noticed. This comes about through delayed closing of the pulmonary valve.
Venous blood should be drawn from the patient and a blood gas analysis performed. Typically, reduced partial pressures of oxygen (pO2) and carbon dioxide (pCO2) are noticeable here. This is usually followed by an imaging confirmation of the suspected diagnosis. Above all, CT or MR angiography and, if necessary, echocardiography or perfusion and ventilation scintigraphy are used. In CT angiography, the pulmonary arteries can be visualized with the aid of contrast media. This method has a high sensitivity for the detection of pulmonary artery occlusions.
Possible radiological signs include the occurrence of Atelectasis (Vacuum areas due to collapse of the alveoli) and pleural effusions. That too Westermark sign (prominent central pulmonary arteries with a noticeable jump in caliber in the periphery), Hampton's hump with a wedge-shaped decrease in transparency in the periphery of the lungs, as a sign of a pulmonary infarction and a Dilation (Enlargement) of the right heart are typical.
When performing a perfusion and ventilation scintigraphy, an imbalance between these two parameters is typically found. While the ventilation (Supply of the lungs via the airways) is usually still completely preserved, the embolus leads to a restricted one Perfusion (Blood supply to the lungs).
Read more on the topic:
- Increased pulse - when is a pulse considered too high?
- Troponin test
therapy
If a fat embolism in the pulmonary or cerebral vessels has been diagnosed, adequate therapy should be initiated as soon as possible.
The main focus is on symptomatic therapy. Inhibition of blood coagulation is possible (Anticoagulation) and the use of glucocorticoids.
However, the use of anticoagulants in particular must be scrutinized, since a fat embolism is not a typical embolus consisting of Platelets (Platelets). Glucocorticoids (such as hydrocortisone or prednisolone) can effectively suppress the inflammatory process in the pulmonary vessels.
Similar topics: Treatment of pulmonary embolism
Additional measures
In addition to these measures, supportive options can also be considered.
Here, the patient can be supplied with oxygen to relieve the shortness of breath or, in the case of complete respiratory insufficiency, mechanical ventilation can be provided.
In the course of the falling blood pressure in pulmonary embolism, it is advisable to give the patient fluid to stabilize the circulation. However, the volume should be administered carefully while monitoring the pulmonary arterial blood pressure using a right heart catheter.
The administration of catecholamines can also stabilize the unbalanced blood pressure situation. The focus here should be on checking the heart rate, as this can already be increased in the event of a pulmonary embolism. The kidney function is also important. In the event of a loss of functionality, appropriate measures must be taken. The symptomatic treatment is usually followed by intensive medical monitoring with further symptomatic care.
What are the long-term consequences?
If a fat embolism is not treated in good time, long-term complications can arise. Since the right heart has to constantly pump against this increased resistance in the case of an acute blockage in the pulmonary vessels, right heart failure can set in if the symptoms persist for a long time. Repeated fat embolisms can also occur after a single incident.
The occlusion of arterial pulmonary vessels reduces the exchange between air and oxygenated blood. As a result, alveoli can collapse and evacuate spaces arise (atelectasis), which can persist over a long period of time. The formation of these atelectases is due to the reduced production of surfactant, which reduces the surface tension of the alveoli during exhalation and keeps them open. The closure of small arteries can lead to a pulmonary infarction, which is mainly wedge-shaped. Then from this infarct area a Pneumonia develop.
You might also be interested in these topics:
- Infarct pneumonia
- Heart failure therapy
Can this be fatal?
The acute onset of a fat embolism can be fatal, even if it is rare, as mentioned above.
The occlusion of the pulmonary vessels can, for example, lead to a worsening of the weak heart and to right heart failure in the case of pre-existing right heart failure.
But especially the rarer occlusions of a cerebral artery can cause life-threatening complications. The stroke with neurological symptoms should be mentioned in particular. The aim here is to restore the blood flow to the closed vessel as quickly as possible.
Also read our topic: Signs of a stroke