Brain tumor
General
As in other organs in the body, benign or malignant growths can also form in the brain.
Every year around 8,000 people in Germany develop a primary brain tumor. These are the lumps that come straight out of the brain.
In addition, there is the multitude of brain metastases, so-called secondary brain tumors.
Some brain tumors typically appear in childhood and are the second most common cancer and leading cause of cancer-related death in children.
Others mainly occur in old age.
The following text explains which symptoms arise as a result, how the brain tumors are classified, which diagnostics are used and how they are treated.

classification
Brain tumors can be divided into benign (benign) and malignant (malignant) growths. This is done by taking a sample from the tumor tissue. In addition, they are differentiated according to the tissue from which they originated, the so-called original tissue, their cell composition and their growth behavior. This classification comes from the World Health Organization (WHO) and includes a total of 130 different tumors of the central nervous system.
There are four different degrees of differentiation:
- WHO grade I: benign, slowly growing
- WHO grade II: still benign
- WHO grade III: already malignant
- WHO grade IV: very malignant, extremely fast growing
The most common primary brain tumors are the meningiomas with around 35 percent, which originate from the meninges. This is followed by the tumors of the supporting cells of the brain (glial cells), the so-called gliomas. These include astrocytomas, ependymomas and oligoendrogliomas, all of which are benign. Ependymomas are growths that start from the inner lining of the chambers of the brain. The malignant glioma includes glioblastoma, which is the second most common brain tumor at around 16 percent.
Pituitary tumors, i.e. tumors of the pituitary gland, make up about 13.5 percent.
This might interest you: These symptoms indicate a pituitary tumor!
The most common brain tumors in children are benign astrocytomas (almost 40 percent) and medulloblastomas. Medulloblastomas are tumors that affect the cerebellum.
In addition to primary brain tumors, i.e. tumors that arise directly from brain tissue, there are secondary brain tumors. These are brain metastases that represent settlements (daughter ulcers) of other malignant tumors from other organs. The new tissue formations in the brain are metastasized with 20 to 30 percent. Predominantly cancers such as skin cancer, kidney cancer, breast cancer and lung cancer often spread to the brain and settle there metastases.
The benign brain tumor
In addition to malignant tumors, there are also brain tumors that can be classified as benign.
These are classified as Grade I in the WHO classification of brain tumors (benign) and grade II (semi-benign) summarized. Benign tumors usually do not grow into other brain tissue and do not destroy it. However, due to their size and the associated compression of the brain, they can be dangerous.
- Tumors that fall into grade I of the classification usually grow very slowly and can in principle be cured by surgery. Whether an operation is possible in an individual case depends on the type and classification of the tumor as well as other factors.
- Tumors, which are classified according to Grade II of the WHO classification, also grow slowly, but have a tendency to reappear and become larger when removed. Nevertheless, these tumors are also often treated with the help of an operation.
Although surgery is the focus of benign tumors, there are indications to treat them with radiation therapy or, more rarely, chemotherapy.
Which individual therapy is possible should be discussed with the attending physician.
You might also be interested in this topic: Brain cysts
The malignant brain tumor
Malignant brain tumors are called malignant because, in contrast to benign tumors, they usually grow very quickly and can grow unhindered into all areas of the brain.
Here, the cells in which the malignant brain tumor grows are destroyed.
The World Health Organization (WHO) divides brain tumors into a scheme that expresses the malignancy of the disease. There are a total of four different levels, with grade III classified as semi-malignant and grade IV as malignant.
Tumors that can be classified within Grade IV usually take a rapid and fatal course.
In addition to the tumors that primarily arise in the brain, there are tumors that occur as metastases (brain metastases) of other malignant tumors in the body in the head.
These are also classified as malicious.
Overall, malignant tumors have an unfavorable to very unfavorable prognosis. However, there are therapies that can significantly extend the life of those affected. Modern chemotherapies in particular, as well as radiation of tumors, can extend the life span. Surgery can also help extend life. Which therapy makes sense in the individual case depends on a large number of different factors and should be discussed with the attending physician.
Read more on the topic: Malignant tumors
Cell-specific tumors
Glioblastoma
Glioblastoma is the term used to describe tumors that originate from certain glial cells, the so-called astrocytes, and that show the most severe "degree of malignancy". They are the most common malignant tumors of the nervous system and have a very poor prognosis. They usually occur between the ages of 60 and 70. In addition, men are affected twice as often as women. Glioblastomas can develop anywhere in the brain, so the specific symptoms can vary widely.
The therapy of glioblastoma consists in most cases of an operation with subsequent radiation and chemotherapy. However, since the tumor grows very infiltratively into the surrounding tissue, not all tumor cells can usually be removed, which drastically lowers the prognosis. The mean survival time after initial diagnosis is between 17 and 20 months.
Read more on the topic:
- Course of a glioblastoma
- Life expectancy with a glioblastoma
Medulloblastoma
A medulloblastoma is a malignant tumor of the cerebellum that usually occurs in children between the ages of four and nine years. It arises here at the attachment point of the cerebellum and from here usually infiltrates both cerebellar halves and the surrounding tissue.
From the described destruction of the surrounding tissue, the typical symptoms of a medulloblastoma follow, to which, due to the involvement of the cerebellum, primarily the ataxia with intention tremor belongs. This describes a motor disorder with increasing tremors during targeted movement.
Other symptoms pose:
- Strong headache
- nausea
- Vomit
- occasionally seizures
- or changes in personality.
The extent of the symptoms depends largely on the size of the tumor. The treatment consists of a complete surgical removal of the tumor, which is usually completed by a subsequent irradiation. The 10-year survival rate for a medulloblastoma is 60%. The prognosis depends on the age of the child. The older the child is at the time of the initial diagnosis, the better the chances of recovery.
Read more on the topic: Medulloblastoma
Meningioma
Meningiomas are one of the most common types of brain tumors with 15%. They arise from the cells of the so-called meninges, the soft meninges. 80-90% of meningiomas are classified as benign, which dramatically improves the chances of recovery. They are known as "pleomorphic". This tumor almost exclusively affects adults. The frequency peak is between the ages of 40 and 60.
Most meningiomas grow very slowly and only displace the surrounding tissue, in contrast to the destruction of the surrounding tissue in "malignant" tumors. As a result, the symptoms usually only appear when the tumor is already large.
Depending on the localization, the spectrum of symptoms includes general signs of an increase in intracranial pressure such as:
- a headache
- nausea
- Vomit
- Visual field loss
- Seizures
- motor disorders
Treatment of a menigeoma, unless there is a contraindication, always consists of surgical removal. If this is not possible due to a complicated situation, for example, radiation is the best possible alternative. The prognosis depends largely on the histology of the tumor, which means whether it is a "benign" or "malignant" tumor. With the more common benign meningiomas, the prognosis is usually good. However, there is also a risk of recurrence of up to 20%. Malignant meningiomas have a significantly poorer 5-year survival rate and 78% of patients will experience at least one recurrent tumor within the next 5 years.
Read more on the topic: Meningioma
Astrocytoma
The term astrocytoma is derived from the original cells of this tumor, the so-called astrocytes. These are part of the supporting tissue of the brain, the so-called glia. This shows that the astrocytoma belongs to the glioma. They make up around a quarter of all brain tumors. The WHO distinguishes between 4 different tumor grades.
The symptoms of an astrocytoma usually only indicate a general increase in intracranial pressure. If there is a suspicion, imaging in the form of CT or MRT is always required. Therapy and prognosis are based on the “degree of malignancy” of the tumor. In the case of grade 1 astrocytoma, for example, after surgical removal, in contrast to grade 3 and 4, no subsequent radiation therapy or chemotherapy is carried out. In addition, grade 1 generally has a good prognosis. In contrast, the average lifespan for a grade 4 astrocytoma (glioblastoma, see below) is only around 18 months.
Read more on the topic: Astrocytoma
Oligodendroglioma
Oligodendrogliomas are classed as gliomas and in most cases are benign. '
They occur mainly between the ages of 25 and 40. Depending on the "malignancy" of the tumor, 4 different degrees are divided.
As with most brain tumors, the symptoms consist of signs of a general increase in intracranial pressure (headache, nausea, confusion), but epileptic seizures also occur more frequently.
The therapy, like the prognosis, of the oligoendroglioma depends on the degree of the tumor and can include chemotherapy and radiation therapy or an operation. The 10-year survival rate for a rather benign and well-located tumor is around 50%. However, this decreases to 20% in grade 4 oligoendroglioma.
Ependymomas
Ependymomas arise from the so-called ependymal cells. In their entirety, these form a layer of cells between the nerve cells and the surrounding cerebral fluid (liquor).
The therapy usually consists of a surgical procedure to reduce the tumor burden, and the tumor can also be irradiated. In general, however, a poor prognosis is pronounced for ependymomas, as these can quickly spread via the CSF into the CNS if they are “malignant”. Thus, the therapy usually only follows a life-extending intention, as a curative (healing) approach. The 5-year survival rate is given as about 45% across all grades. The therapy usually consists of a surgical procedure to reduce the tumor burden, and the tumor can also be irradiated.
Pituitary tumor
The mostly benign pituitary tumors arise from hormone-producing cells in the pituitary gland, which regulates large parts of the human hormone balance. In pituitary tumors, a basic distinction is made between hormone-producing (active) tumors and those that do not produce hormones (inactive).
The symptoms of active pituitary tumors can be very numerous due to the influence on the endocrine system. These include missed periods, possible breast enlargement in men, osteoporosis (decreased bone density), changes in height, the development of a bull's neck and many more.
In addition, with these tumors it is important to ensure that the pituitary gland is close to part of the visual pathway, the so-called optic chiasm. Above a certain size of the tumor, compression of this visual pathway can lead to visual field defects. The therapy of the pituitary tumor usually consists of a surgical procedure that can be carried out through the nose. The prognosis is very good due to the “benign nature” of the tumor and the good surgical access.
Read more on the topic: These symptoms indicate a pituitary tumor!
Schwannoma
Schwannoma, also called neuroma, is a benign tumor that originates from so-called Schwann cells. These cells are found all over the peripheral nervous system, but schwannomas tend to develop in two specific locations.
On the one hand, schwannomas arise from parts of the cranial nerve that is responsible for hearing and the sense of balance (vestibulochochlear nerve). In this case, the schwannoma is called an acoustic neuroma.
The other common location is the sensitive nerve roots in the spinal cord. Depending on the localization, different symptoms occur. In the case of an acoustic neuroma, most of those affected initially report a hearing loss, which increases as the disease progresses. In addition, tinnitus (ringing in the ears) or dizziness can occur.
If swans appear on the spinal nerves of the spinal cord, symptoms of paralysis, sensory disorders or radiating pain can occur. Different therapy options are available depending on the size of the tumor. If the swan is still small, targeted irradiation can be considered. Most swan tumors, however, are completely surgically removed, which leads to healing.
Read more on the topic: Neuroma
Neurofibroma
Neurofibromas are benign nerve tumors that can grow in or outside of a nerve.
Some of them also consist of Schwann’s cells, but are characterized by a schwannoma because they cannot be separated from the nerves. Thus, when a neurofibroma is surgically removed, the affected nerve is usually also lost. Basically, neurofibromas can occur anywhere where there is nerve tissue. However, they occur more frequently on the skin.
People with the genetic disease neurofibromatosis 1 can have hundreds of small neurofibromas that cannot be removed without scarring. For the therapy of neurofibromas on the skin, lasing with a carbon dioxide laser has become established.
Read more on the topic:
- Symptoms of neurofibromatosis type 1
- Neurofibromatosis 2
Hemangioma
A hemangioma (also called a blood sponge) is a benign tumor that affects blood vessels and occurs primarily in childhood.
Two thirds of hemangiomas develop in the head and neck area. Hemangiomas diagnosed in children are usually congenital. However, there are also non-congenital hemangiomas, which usually only develop in adulthood.
Hemangiomas can develop anywhere where there are vessels, including in the brain. If a wait-and-see therapy option is often chosen in other areas, such as the skin, since hemangiomas can regress on their own, the decision in the case of hemangiomas in the brain depends largely on their size and symptoms. In addition to dizziness and headaches, other neurological deficits can occur, which can be a sign of an insufficient supply of the nerve tissue with oxygen. Therapy then usually consists of radiation, embolization (closure of the hemangioma with a catheter) or surgery.
Also read our topic: Cavernous Hemangioma - How Dangerous Is It?
Hemangioblastoma
Hemangioblastomas, or angioblastomas for short, are benign tumors that occur in the central nervous system.
They usually arise in the spinal cord or in the posterior fossa. The development of a hemangioblastoma is usually associated with the growth of a cyst, as this can be part of the firmer outer layer.
These tumors form what is known as erythropoietin (EPO for short), which increases the production of red blood cells. Depending on the localization, further symptoms can occur. If the hemangioblastoma is in the cerebellum, for example, movement disorders, dizziness, nausea and headaches can occur. However, since these tumors usually only grow slowly, a wait-and-see procedure is usually chosen first. Once the tumor has reached a critical size, it can usually be completely removed by surgery.
Causes and Risk Factors
The exact Causes of the development of brain tumors are to this day largely unknown. Apparently there is several factorswho participated in the making of Brain tumors could be involved:
- Genetic causes:
certain rare hereditary diseases, such as: the Recklinghausen's disease in the Neurofibromatosis, the Turcot Syndrome, the Hippel-Lindau syndrome as well as that Li Fraumeni Syndrome can increase the risk of developing a brain tumor. - By a radiotherapy, which is used to treat many types of cancer, carries the risk of brain tumors occurring more frequently.
- Also the increasing age As with other cancers, it is associated with an increased risk. This is especially true with glioblastoma.
Other possible causes such as environmental toxins, Eating habits, emotional stress, stress and electromagnetic waves generated when talking on a cell phone are discussed. According to the current state of knowledge, however, there is no context.
Symptoms
A distinction has to be made between slow and fast growing brain tumors. The slowly growing demonstrate the appropriate complaints only late. Fast growing, however, space-occupying cancers show the corresponding symptoms quickly on.
Especially so-called occur Intracranial pressure sign on. They arise from the fact that the cancer displaces the healthy tissue in the brain and leaves no more room to evade, as the bony skullcap cannot expand any further. This is how a increased pressure in the brain. The intracranial pressure signs include:
- a headache
- Disorders of consciousness (Drowsiness to the coma)
- Seizures
- such as nausea and Vomit.
In itself is a headache mostly harmless. If they occur again, especially at night and in the morning, more severe, more frequently than usual and if they keep coming back, a doctor should be consulted.
Furthermore can neurological failures occur, these are noticeable through:
- dizziness
- Paralysis
- Visual and sensory disorders
- Balance disorders
- Unsteadiness
Also are mental changes (easily irritable, more distractable) and abnormal behavior is possible.
In children, especially infants in the first year of life, whose cranial sutures have not yet been closed, the increased intracranial pressure leads to the individual skull plates diverging. This manifests itself through a Bulging of the bony gap of the skull and a strong head growth.
You can find further information under our topic: Brain tumor signs.
Signs of a brain tumor
A brain tumor initially grows mostly undetected within the skull.
However, depending on the location, size and type of the tumor, certain symptoms can occur, which are to be assessed as signs. If certain signs are noticed, it is therefore advisable to have the symptoms clarified by a doctor. This can use diagnostic methods to find out whether it is Signs of a brain tumor or whether the symptoms are due to other diseases.
In general, a distinction must be made between signs that arise solely from the increasing mass of the tumor and signs that are caused by damage to certain brain cells.
Furthermore, certain signs arise that can be attributed to the presence of a malignant tumor disease.
The space inside the skull is generally limited, which is why it becomes larger tumor there is a lack of volume within the skull.
Usually in the course of this volume increase there is one Irritation of the meninges. These are, in contrast to the brain yourself, sensitively cared for. In the case of brain tumors, the first sign is usually severe a headache which partly with Vomit accompanied.
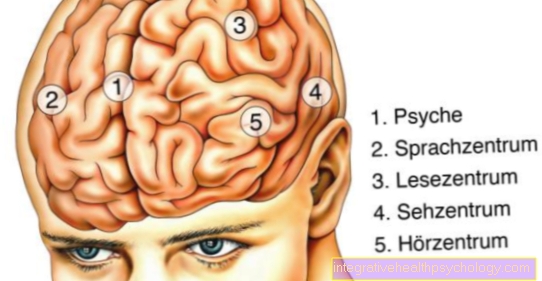
The signs that are caused by the direct irritation of certain areas of the brain can be very different.
Tumors in the area of the optic nerve can restrict the field of vision. It can also Signs of paralysis or Disturbance of smell, Swallowing, Listening or Tasting occur.
Areas that influence the hormonal balance in the body are sometimes irritated. If you suddenly have seizures or have difficulty concentrating, or if your personality appears to be changing, this may also be due to a brain tumor.
Signs that can arise in many tumor diseases and also in a number of brain tumors affect the entire body. Night sweats, weight loss and an inexplicable fever are typical reactions of the organism to the disease.
diagnosis
If a brain tumor is suspected, a thorough medical history (consultation with the patient) should first be carried out, followed by a detailed physical and neurological examination. Imaging methods should then be used to determine the exact location of the tumor. The most important procedures here are magnetic resonance tomography (more precisely magnetic resonance tomography head) and computed tomography (CT) of the head. During these examinations, sectional images of the brain are made, on which practically all brain tumors are visible.
A puncture of the cerebral fluid (the so-called liquor puncture) can in certain cases indicate a tumor in the brain.
The attending physician often orders a positron emission tomography (PET) of the head. This allows you to get information about the sugar metabolism of the tumor and tell whether it is a benign change (e.g. a scar or an inflammation) or something malicious. In addition, a PET can be used to make a statement as to whether it is a slowly growing benign or a rapidly growing, malignant tumor.
Read more on the topic: Positron emission tomography
A tissue sample is necessary to make a 100% reliable diagnosis of the brain tumor and the type of tumor. This can be done during the surgical removal of the brain tumor or separately via a small operation.
As already mentioned, the tissue sample can be used to divide the tumor into grades I to IV according to the WHO classification:
- Grade I: This is where the benign tumors are located, which grow only slowly and differ only slightly from normal tissue cells.
- Grade II: These are still benign tumors that grow into the environment. This is also known as infiltrative growth. A further development towards more aggressive tumors is possible.
- Grade III and Grade IV: The tumors grow rapidly to extremely quickly and show signs of malignancy in the tissue sample.
therapy
The therapy depends on the exact location of the brain tumor and the type of growth. Therefore, the result of the brain biopsy (sampling) must be awaited.
Read more about this topic here: biopsy
After a precise diagnosis, the brain tumor can be treated in different ways. This includes first of all the surgical removal of the tumor by the neurosurgeon. Radiation of the tumor (radiation therapy) and chemotherapy are also included.
In addition to these three classic options, other treatment concepts and modern approaches are available that are currently being tested in various clinical studies or are also being used as an individual healing attempt.
Before starting therapy, however, it is important to inform the patient about the possible advantages and disadvantages and to report on alternatives. In some cases, waiting and observational treatment is chosen, as the above-mentioned forms of therapy do not promise greater success in certain stages. The individual therapy options are explained in more detail below.
surgery
The surgical removal of a brain tumor is carried out by Neurosurgeons made after a accurate diagnostics was carried out. It is important to know the exact location of the tumor, the condition and symptoms of the patient in order to be optimally prepared for the operation.
Depending on the size and location different access routes elected. There is direct way, in which the surgeon opens the skullcap with a special saw or introduces the instruments through a drill hole in the skullcap. This is called transcranial access designated. Furthermore, there is the possibility, if the tumor location allows, through the nose to carry out the removal of the growth.
Brain tumors can be removed as far as possible by surgery, but they can also only be partially removed.
It is also possible that the neurosurgical treatment cannot be carried out at all. Of the tumor is therefore inoperable and can through a so-called partial Brain amputation cannot be removed. This is particularly the case when the tumor is located directly in an area that houses important functions of the human body that would be severely impaired or even destroyed by an operation. Since such interventions always run the risk of removing healthy nerve tissue and thereby causing neurological disorders such as Memory problems, Signs of paralysis, Speech disorders or Unsteadiness, imaging tests such as MRI and CT are often used during surgery.
In some brain tumors, the navigated brain stimulation or a intraoperative language monitoring be useful. Usually, surgery is the only treatment needed for benign brain tumors. Further methods are used for tumors with an increased risk of relapse (i.e. from WHO grade II), for tumors that have only been partially removed or for inoperable brain tumors.
Surgery for a brain tumor
The operation of a brain tumor can be useful or necessary for different reasons.
A distinction must be made between different indications for performing an operation. For example, benign brain tumors can be cured with surgery.
Malignant brain tumors can rarely be cured with surgery. Nevertheless, an operation can improve the quality of life or extend the life span.
Surgery is also required to collect samples to identify specific tumors. Some tumors can only be clearly identified under the microscope. The determination is important for the creation of an individual therapy concept.
Surgery for a brain tumor is performed by specially trained neurosurgeons.
During the operation, the skull is opened and special tools are used to prepare the way to the tumor. During this time, the affected patient is usually under general anesthesia.
If certain regions of the brain have to be manipulated, only a local anesthetic is sometimes performed so that important regions of the brain can be spared during the operation. In both cases, the affected patient does not feel the intervention.
radiotherapy
Radiation of tumors can be used before (neoadjuvant) and / or after (adjuvant) the surgical removal and as the sole treatment. The high-energy radiation from photons or electrons, for example, is used to To prevent tumor cells from growing or the To disrupt the cell division process. Because diseased tissue reacts more sensitively to radiation therapy than healthy tissue does mainly the tumor tissue destroyed.
Radiation therapy can be carried out externally as well as via certain radiation sources (e.g. radionuclides) that are placed directly in the tumor area of the brain. However, this can also lead to neurological failure symptoms. The irradiation is either fractionated, i.e. carried out in several individual sessions, or applied as a single therapy.
chemotherapy
With this treatment come so-called Cytostatics to use that prevent diseased tissues from dividing and the Tumor to death bring.
With this type of therapy, the rapid division of the brain tumor cells is used, as such cells are more sensitive to chemotherapy. Unfortunately, healthy cells in the body, which also divide quickly, are also damaged. So it can too certain side effects how Hair loss or Changes in blood count come.
The chemotherapy is clustered in Combination with radiation therapy carried out. Then one speaks of one Chemoradiotherapy.
The same neurological problems as with surgical therapy can occur as side effects. In this therapy, the drugs (cytostatics) are administered directly into the blood or swallowed (orally) as capsules. Exactly which drugs are used depends on the type of brain tumor.
Then some cytostatics that are used for brain tumors are listed: Cisplatin, Vincristine, Fluorouracil (5-FU), Irinotecan (CPT-11) and many more are used for treatment.
Summary
In order for brain tumors to be detected and treated early enough, you should Always consult a doctor if you have the following symptoms:
- increasingly strong a headache, especially at night or in the morning
- dizziness With nausea and Vomit
- Loss of consciousness
- Balance disorders
- sudden changes in vision or Visual field loss
- Language problems
- Sensory disturbances
- sudden Signs of paralysis
- a first-time appearance epileptical attack.
If you have noticed the above symptoms in your child or another person, you should also see a doctor with them as soon as possible. As soon as a brain tumor has been diagnosed, psychosocial support for the patient and their relatives is advisable.























.jpg)