OP of an intestinal obstruction
introduction
With an intestinal obstruction (Ileus) comes the forward movement of the intestine (peristalsis) due to mechanical or functional causes to a standstill. The intestinal contents build up and lead to severe symptoms, such as vomiting of feces. A bowel obstruction is a potentially life threatening situation that must be treated as an absolute emergency in a hospital. The faster an intestinal obstruction is treated, the fewer the complications associated with it. In addition to conservative treatment options such as placing an enema, immediate surgical treatment of an ileus is the method of choice.
Read more at:
- Intestinal obstruction
- Acute abdomen

The surgical procedure
Preparation for the operation
Before the ileus operation, the patient learns about the procedure and the risks of the operation in an informative discussion by the doctor. This conversation is not necessary in an emergency. The location of the ileus can be determined before the operation by an X-ray examination or an ultrasound.
Many medications that are taken regularly must be paused. Anticoagulant drugs such as heparin or Marcumar must also be discontinued before the operation so that the risk of bleeding does not increase. To stabilize the general condition, the patient receives an infusion to replace electrolytes. In addition, the patient must be sober for the operation and have received premedication (sedative medication).
What happens during the operation?
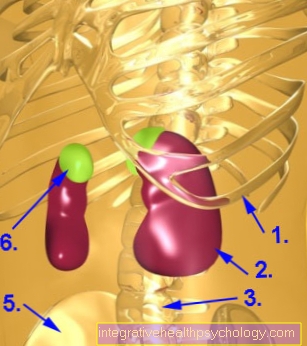
The operation of an intestinal obstruction is a major procedure that takes place under general anesthesia. After the skin has been sufficiently disinfected, the surgeon makes a straight incision in the middle of the abdomen at the level of the navel (median laparotomy). The height of the incision can vary and depends on the suspected location of the ileus. Then the skin and muscle layers are spread and access to the abdominal cavity is opened.
After the surgeon has visited the affected intestinal incision, he can remove any adhesions or bring the clamped or twisted parts of the intestine back into the correct position. If parts of the intestine are already so badly damaged by the lack of blood supply or a tumor that they will no longer recover, they must be removed. To do this, the damaged section of the intestine is clamped and cut out. This procedure is known as bowel resection. Then the two remaining intestinal stumps are sewn or stapled together. If the intestine has already been perforated by the congestion and intestinal contents enter the abdominal cavity, the abdominal cavity must be thoroughly rinsed with germicidal solutions, otherwise the bacteria will cause peritonitis. At the end of the operation, the abdomen is rinsed and the cut open muscle and skin layers are sutured again.
Most often, an artificial anus is used after an intestinal resection (Anus praeter) to allow the intestinal lining to heal. To do this, a loop of the small intestine, which lies in front of the sewn section, is pulled through an incision in the abdominal wall and fastened there (double-barreled stoma). The contents of the intestine are emptied via the stoma into a bag that is glued over the anus praeter and must be changed regularly. This can be done by yourself or by qualified personnel. After a few weeks, the wound caused by the partial resection has healed and the artificial anus can be moved back.
Duration of the operation
The ileus operation is a major procedure that can take several hours. The exact duration of the operation depends on the cause of the intestinal obstruction. Kinks and tangles can be removed relatively quickly and the bowel can be repositioned in its original position. The surgeon can also remove uncomplicated adhesions and braces within the planned operating time.
However, if a tumor that narrows the intestinal lumen or entire parts of the intestine have to be removed, the duration of the operation is extended accordingly. In many cases, an artificial anus must be created after a bowel resection. However, this is a routine step that can be done quickly.
Aftercare
After the operation, the wound is treated with wound drainage and covered with sterile bandages. The patient then comes to the recovery room, where he wakes up from anesthesia under constant medical supervision. The freshly operated person is then transferred to the ward, where he has to stay for several days.
The patient receives medication that relieves pain and the hospital staff tends to the surgical wound. The patient is not allowed to eat anything for the first few days after the operation and is fed via infusions (parenteral nutrition). Then you can start with light food (soup, porridge, yoghurt, etc.), so that the intestine can slowly get used to food again and begin digestion. It is important that the patient strictly follow the doctor's instructions, as overloading the intestines with unsuitable foods will lead to serious complications and the need for another operation.
Length of hospital stay
As a rule, patients must expect an inpatient hospital stay of at least four days after an ileus operation. If complications occurred during the operation or if entire parts of the intestine had to be removed, the length of the hospital stay is extended. In such cases, patients may need to stay in the hospital for up to two weeks or more.
Duration of total healing
The duration of the entire healing depends to a large extent on whether it is a mechanical or paralytic intestinal obstruction and what caused it. A mechanical bowel obstruction is treated surgically in most cases and is associated with a long hospital stay.
A paralytic ileus must not be operated on, but must be treated conservatively with medication, intestinal enemas and massages. Accordingly, the hospital stay is shorter. Depending on the severity of the intestinal obstruction and whether complications have occurred, healing can take weeks to months.
What are the risks of the operation?
In recent years many new surgical methods have become established, which means that even large operations are associated with fewer risks and complications for the patient. However, like any operation, ileus surgery involves certain risks that cannot be completely prevented.
During the operation, the intestine can tear or be otherwise damaged, which allows bacteria to enter the abdomen and lead to peritonitis. There is also the risk of severe bleeding in the abdomen or other abdominal organs due to vascular injuries.
Please also read: Circulatory disorder in the intestine
The operation on the intestine can lead to adhesions on the intestinal loops in the course of the healing process, which can again lead to an intestinal obstruction. Another risk is that the wound will not heal properly or that a hernia will appear through the abdominal wall.
An ileus operation is a serious procedure that can therefore be associated with many complications. However, an intestinal obstruction is an absolute emergency situation, in which action must be taken quickly, as otherwise it leads to organ failure and can be fatal.
How high the risk of the actual occurrence of these undesirable side effects is primarily depends on the age of the patient, their general condition, accompanying diseases and the cause of the intestinal obstruction. The doctor will explain to the patient extensively about possible risks and complications before the procedure.
Long-term consequences of an operation
The operation of an intestinal obstruction can have long-term consequences. If intestinal tissue is removed during the operation, the risk increases that connective tissue adhesions will form at this point, which will later reduce the diameter of the intestine and lead to another intestinal obstruction.
Especially after the removal of a section of the intestine, the operation can lead to digestive disorders and changes in bowel movements. The symptoms depend on whether parts of the small or large intestine have been removed and how much has been cut out. Most of the time, the stool becomes thinner and more frequent. Patients must pay attention to their diet and adapt it to the new circumstances. Even before the operation, the doctor explains in an informative discussion how the digestion will change as a result of the operation and what consequences the person concerned must expect.
After an intestinal resection, an artificial anus (double or terminal stoma) is often created, which after a few weeks, when the surgical wound has healed, can be moved back into the abdominal cavity. In some cases, the artificial anus has to be permanent. This is especially the case if the large intestine had to be partially or completely removed. In the case of a permanent artificial anus, the remaining section of the small intestine is sutured directly to an exit on the abdominal wall. The contents of the intestine are emptied via a bag that is attached to the abdominal wall.
Can this be fatal?
Intestinal obstruction is a serious condition that can be potentially fatal. Basically, the prognosis depends on how quickly the treatment takes place and how big the affected section of the intestine is. The death rate after the operation is relatively high, around 25%. However, this is mainly due to the fact that the majority of patients are already older and often also have a serious underlying disease, such as a mesenteric infarction or a tumor.
When does an intestinal obstruction need to be operated on?
The method of treatment depends on the type of intestinal obstruction. Only a mechanical bowel obstruction is operated on, whereas a paralytic ileus must not be treated surgically. Treatment of paralytic ileus lies in the elimination of the cause and conservative therapy.
A mechanical ileus is generally treated surgically. Surgical intervention as early as possible reduces the risk of serious complications, such as intestinal perforation or bacterial inflammation of the peritoneum (perotinitis).
Immediate ileus operation is postponed only in a few cases, for example if the general condition of the patient is so poor that the risk of an operation is too high. Then an attempt is first made to stabilize the patient with electrolyte infusions and other circulatory support measures so that an operation is possible.
All important information can also be found at: Treatment of a bowel obstruction
How much intestine may / must be removed
The decision whether and, if so, how much intestine needs to be removed during an ileus operation depends on the cause of the intestinal obstruction. Is it a simple mechanical bowel obstruction with a benign cause, e.g. a clamp due to an inguinal hernia or an intestinal twist, the affected section can simply be returned to the normal position and a section of the intestine can be surgically removed (Resection) is not necessary.
The case is different if a tumor has grown into the intestinal mucosa and causes the blockage. Then the entire part of the intestine that is affected by the tumor must be completely removed. The same applies to a heavily thickened and scarred intestinal wall, which often forms after chronic inflammation. In some cases, the blood supply can no longer be maintained due to the mechanical clamping and parts of the undersupplied intestine die. In such a case, the dead tissue must be completely removed.
Intestinal obstruction as a complication of other operations
About half of all intestinal occlusions are caused by adhesions (Adhesions or clamps). This is proliferating tissue that is formed in the healing process of scars. Operations in the abdomen in particular often lead to scarring and the growth of adhesions. When the adhesions form around a section of the intestinal tube, the diameter of the intestine is narrowed, the intestinal contents build up and a mechanical ileus develops. This clinical picture is called Bridenileus. Various abdominal surgeries, such as appendectomy, hysterectomy or caesarean sections, promote the development of these adhesions, which is why an intestinal obstruction can often arise after a previous operation. Bridenileus is treated surgically by removing the adhesions around the bowel. However, the procedure leads to new scars and the intestinal obstruction can arise again.