Periradicular infiltration therapy
Synonyms
PRT, herniated disc, back pain, CT guided infiltration
definition
The periradicular therapy (PRT) is a pain therapy procedure for one disc prolapse and other back conditions in which a drug is injected into the vicinity of the exiting spinal cord nerves under CT imaging.

introduction
In the Periradicular Therapy (short: PRT) is a drug mixture in the range of a Nerve root injected to relieve the pain associated with the nerve root. The drugs used are usually a mixture of Local anesthetic and Cortisone Preparation.
Explanation

Periradicular therapy (around the nerve) Infiltration therapy (Syringe treatment) is a pain therapy method that is becoming increasingly important.
On behalf of orthopedists, the treatment is carried out in the outpatient area by radiologists (x-ray doctors). In order to achieve the greatest possible effect, a series of 3-6 infiltrations is usually carried out. Billing for this special form of treatment is borne by the health insurance company.
In the inpatient area, periradicular therapy (PRT) is part of the conservative orthopedic treatment options for back pain patients.
In the case of unclear pain syndromes, switching off individual spinal cord nerves can help to prove the actual cause of the pain. Such information is also of great importance for any planned operational procedure.
You might also be interested in: CT-guided pain therapy
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
application
Periradicular therapy can be used for all clinical pictures that lead to painful irritation of the spinal cord nerves. This includes:
- disc prolapse
- Back pain
- Lumboischialgia
- Spinal stenosis
- Facet syndrome
- Degenerative spinal diseases
Periradicular therapy on the cervical spine
As in other areas, the Periradicular Therapy in the field of Cervical spine can be used for variously caused pain conditions. For example at Compressions of the beaten nerves, Nerve damage by Herniated discs of the cervical spine or if there are problems related to a accident, or Scarring after a previous operation.
The therapy can also be helpful for general problems caused by wear and tear.
When treating the cervical spine, one is in the side or prone position. The whole procedure takes place under CT controlso that the attending physician can visualize the area in which the needle is located during the entire procedure.
In most cases, an exact measurement of the affected area is made beforehand using a CT image. By injecting a contrast medium, it can be precisely checked during the treatment whether the target area has been reached. This is particularly important in the cervical spine area, as the nerves exiting here control a large number of vital body functions.
When the doctor has a great deal of certainty in the field of PRT contrast agent administration can be dispensed with in order to increase the speed of the therapeutic measure and to reduce the complication rate.
In addition to the actual periradicular therapy, in which the active ingredient is injected directly at the exit point of the nerve root, there is also the option of performing the treatment in the area of the facet joints.
These are the joints between the lateral parts of the Cervical vertebrae. Especially with wear it occurs more often in these Blockages or Inflammation. The injected cortisone / Hyaluronic acid has an anti-inflammatory effect and prevents a further worsening of the symptoms and has an analgesic effect.
Symptoms generally improve immediately or after 1-3 days. This treatment is usually repeated at intervals of 1-3 weeks, a total of 3 times, in order to achieve permanent relief of the inflammation and long-term inhibition of the pain-processing nerve fibers.
This is the only way to prevent the development of a so-called pain memory and thus avoid or break through chronic pain.
Periradicular therapy on the lumbar spine
Also in Lumbar vertebrae Periradicular therapy is often used in the area. The range of applications here is also primarily in the area of Herniated discs, Entrapment (please refer: Pinched sciatic nerve) and other chronic degenerative changes.
These occur in a particularly large number of people in the lumbar spine area. In old age, this carries up to 70% of the body weight due to the increasing breakdown of normal intervertebral discs.
Different from one PRT in the cervical spine area, the treatment is always carried out in the prone position. Especially in the lumbar region is the Periradicular therapy under MRI control an interesting alternative to the usual CT guided injection. Since the very radiation-sensitive genital organs are located near the lumbar spine in the pelvic area, a particularly radiation-saving approach should be used with younger patients in particular.
Also the treatment of the facet joints as well as the so-called Epidural Therapy are possible in the lumbar region.
With epidural therapy, not just a single nerve root is treated. Instead, the active ingredient is above the Dura mater (hard meninges) placed in the area between the spinal cord and bone.
This is especially beneficial when multiple nerve roots are affected. As in the other areas of the spine, periradicular therapy can only bring about symptom relief in the lumbar region. It does not combat the actual cause. However, the anti-inflammatory effects will slow down further deterioration and allow the body to heal part of the defect.
Due to the radiation exposure described above, when performing CT or X-rays, it should always be considered whether other methods of pain relief are also possible, especially in the lumbar region.
background
In the periradicular therapy (PRT) are under computed tomography (see CT) or radiographic position control, analgesic and anti-inflammatory drugs (anesthetic / cortisone mixture) are administered to the painful nerve root with millimeter precision. Usually a Cortisone injection used.
Please also read our page Cortisone in a herniated disc.
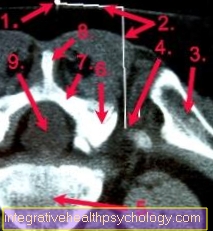
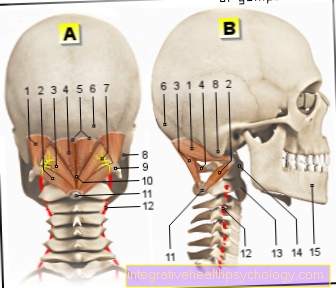
PRT
- Orientation wire on the back surface
- Infiltration planning: depth and lateral distance to the orientation wire
- pool
- Nerve root exit 1. Sacral root (S1) right
- Vertebral bodies
- Vertebral joint
- Vertebral arch (lamina)
- Vertebral spinous process
- Spinal canal
The figure shows a CT-guided periradicular therapy the first sacral root (S1) on the right, which is particularly common Herniated disc of the last lumbar disc (L5 / S1) gets irritated. By a PRT the inflammation around the nerve root is contained and the nerve root becomes swollen. In the case of herniated discs, shrinkage of the displaced disc tissue can sometimes be observed.
Several such infiltrations are often necessary to achieve the desired therapeutic effect. Due to the swelling of the nerve root, there is relatively more space in the nerve exit area Spine.
And although constricting bone edges or a herniated disc of the lumbar spine or Cervical spine continue to exist, freedom from pain can be achieved.
In addition, the anti-inflammatory effect of the cortisone means that the nerve root no longer reacts so sensitively to mechanically or chemically irritating stimuli (e.g. intervertebral disc tissue).
The intervention is not a substitute for surgical therapy, but can be used as an alternative to immediate surgery in the case of therapy-resistant pain with no or only minor neurological failures.
The use of the Computed Tomography is not absolutely necessary for an injection treatment, an image converter (mobile X-ray device) supported infiltration open MRI and even infiltration without imaging are possible.
In the latter case, one orientates oneself on certain body points (anatomical landmarks). If a sufficiently large infiltration volume is selected, an almost exact placement of the syringe is sufficient, because the administered active ingredients are distributed in the environment and the pressed nerve root can nevertheless effectively flood.
An exact procedure with the CT (Computed Tomography) as an imaging method is nevertheless recommended, especially if the infiltrations are to confirm a diagnosis.
The pain therapy effect is very good. The infiltration can be repeated several times, has few complications and can be carried out on an outpatient or inpatient basis.
A anesthesia is not necessary.
Action

The patient is placed on his stomach on the computed tomography table. The arms are placed forward under the forehead. Then a metal orientation wire is glued to the middle of the (mostly) lumbar spine on the bare back. (Periradicular therapy is also suitable for nerve root irritation in the cervical and thoracic spine).
Finally, the CT (computer tomography) is used to take an overview of the relevant back region. The doctor can then use this image to determine the location of the pathological nerve root. This area is then exactly represented with the CT (computer tomography). Once the desired nerve root origin has been determined, the infiltration depth and the lateral deviation from the center of the spine are determined for the infiltration. The previously glued-on wire, which is visible as a point on the CT cross-sectional image on the patient's back, serves as a guide. A strip of light, which is projected onto the patient's back, shows the doctor the level of infiltration.
The determined lateral deviation from the orientation wire is measured with a ruler and marked on the skin. After the skin has been disinfected, the needle (cannula) is positioned. The predetermined path to the nerve root is pierced with a cannula that takes into account the depth of infiltration. In order to confirm the correct placement, the position of the cannula tip to the nerve root is shown again in the CT (computer tomography). If the needle tip is correct, the mixture of a local anesthetic and cortisone is injected as described above. If the doctor deviates from the placement of the cannula, the cannula position must be corrected and checked again.
After the infiltration, the patient should lie down for 2 hours if possible. A leg weakness due to the nerve block is possible.
Complications
Various complications can arise from periradicular therapy, which in drug-induced A distinction must be made between complications and technical complications. As for the exact localization of the Injection site a Contrast media must be applied, incompatibilities may occur. These express themselves in the context of a allergic reaction and can from Reddening of the skin, nausea and dizziness to unconsciousness pass. However, this complication is rare.
In addition, contains the applied drug cortisonewhich has various side effects. This includes an increased Facial flushing, sweat, Calf cramps, Stomach discomfort, as well as a Rise in blood sugar and pressure. Should these complications occur, they can be treated well with additional medication.
You can do the surgery yourself Bleeding and Infections occur as germs can be carried into the wound from outside. Forms in the area of the nerves Hematoma or if a massive infection spreads there, they are permanent paralysis and depend on the injection site Paraplegia possible. However, this is a very rare complication. Furthermore can Nerve injuries occur when the doctor performing the procedure hits a nerve with the needle. This can be massive Pain and at times also to Paralysis in the leg to lead. However, these complications are usually reversible because the needle can only slightly injure the nerve. Temporary symptoms of paralysis can also occur as a result of the application of the anesthetic and are relatively common. However, when the anesthetic is broken down, the paralysis disappears. If the anesthetic is mistakenly placed in the Dural sac injected, the paralysis can be much more pronounced and long-lasting, but this paralysis is also reversible.If temporary paralysis occurs after the therapy, it is no longer fit to drive.
Risks
Theoretically are
- Injuries to the nerve root
- Bleeding
- bacterial inflammation
- allergic reaction to the medication
possible. A certain period of post-infiltration monitoring should be observed.
Since periradicular therapy is a invasive Intervention, some risks are possible. For this reason, the patient must be informed about the existing risks and a written declaration of consent submit. Since periradicular therapy is an intervention, are Infections and Bleeding always possible. However, these risks are through sterile Work and that minimally invasive Minimize procedures. However, these complications do occur in some cases. When forming a Hematoma or spread of infection in the nerve root area Signs of paralysis possible. In most cases, these are reversible, but in exceptional cases the paralysis persists.
In addition, other structures such as nerves or ligaments and muscles in the area of the injection site can be injured during the positioning of the needle. Because of the CT-controlled Procedure and thus constant control of the position, these risks are very low. During the examination, the patient is given a Contrast media administered through the vein to expose the structures. This calls in some cases allergic reaction which can be seen in the form of dizziness, itching, Redness or even one allergic shock can express.
Furthermore, the patient is injected with various drugs in the area of the nerve root. These drugs contain, among other things, cortisone, which has an anti-inflammatory effect. However can cortisone Influence on the Blood sugar and the Blood pressure to take. Because of this, are diabetic or patients with a high blood pressure more at risk of being affected by these risks. By injecting the Local anesthetic In many cases, a temporary weakness of the affected muscles occurs. For this reason, the driver is not fit to drive within the first 6 hours after the therapy. If the medication is mistakenly injected too deeply into the dural sac, more severe and longer lasting paralysis is possible. However, these symptoms of paralysis are usually fully reversible after absorption of the drug. In the worst case scenario, depending on the injection site, the drug can cause an injection that is too deep Respiratory paralysis cause.
Side effects of periradicular therapy
To the Side effects of periradicular therapy First of all, there is the not inconsiderable radiation exposure, especially in the lumbar area, and the resulting risk.
Furthermore, the injections themselves can cause complications. First of all, there is always the risk of one allergic reaction on the drugs or contrast media used.
The cortisone used, especially with frequent use, can lead to side effects such as fragility of small vessels, rise in blood sugar or menstrual disorders in women.
The puncture itself carries the risk of damaging the nerves or the spinal cord. The invasive penetration can also lead to bleeding or infections. However, this is very rare due to the X-ray control. After the treatment, there may be temporary sensory disturbances in the legs, as well as burning and pain at the injection site.
If the anesthetic gets into the spinal canal, temporary paralysis of the legs can occur. Also nausea, Headache, dizziness and high blood pressure are possible immediately after the treatment.
However, these usually occur immediately after the treatment, i.e. still under medical supervision, and usually improve quickly.
Cost of periradicular therapy
Since the effect of the Periradicular therapies So far it has not been scientifically proven that most of the statutory health insurance companies no longer cover the costs.
Some health insurance companies have special offers or partnerships with certain practices, so that reimbursement may not be possible at the doctor of your choice, but in certain centers.
In any case, it is worth making an inquiry with the health insurance company itself. Often it is also a prerequisite that the referral for treatment, or the implementation itself, is arranged or carried out by a specialized pain therapist.
A Treatment of herniated discs is usually not accepted. In general, the periradicular therapy must be integrated into a so-called multimodal, i.e. comprehensive pain concept consisting of different approaches. Many practices therefore offer periradicular therapy as a IGEL performance so for self-payers.
The costs are around € 100-250 per injection, for the actual treatment, depending on the location and difficulty of the puncture.
However, the costs for the necessary CT images are usually added here.