Peroneal tendon dislocation
definition
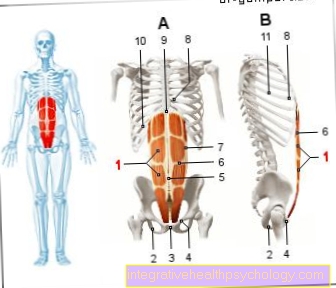
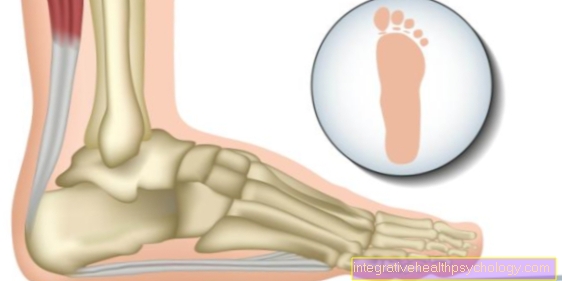
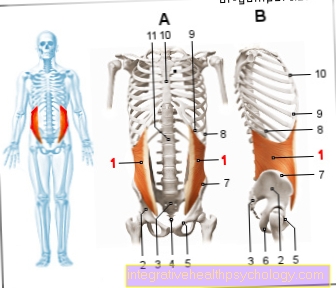
At a Peroneal tendon dislocation It is a rather rare injury in which the tendons that connect the lateral lower leg muscles to their attachment points on the foot slip out of their normal anatomical position. The peroneal tendons run along the side of the foot, coming from the lower leg, behind the outer ankle and are held in place by a small additional strap. If this ligament is damaged due to injury, the tendons slide forward. It comes to Peroneal tendon dislocation, which are also classified as chronic habitual Form can occur.
You can find more information about the Peroneal tendons.

Symptoms
A Peroneal tendon dislocation causes a number of typical symptoms. Due to the incorrect position of the tendons in front of the outer ankle, you can see a bulging and swelling there, which is also caused by a slight inflammatory reaction. At this point the peroneal tendon dislocation can be felt from the outside. You can feel a sinewy structure that lies under the skin and slides under your finger when you move your foot slightly. You may feel the tendons snap over the bone. Additional symptoms of peroneal tendon dislocation are pain and instability. The pain occurs mainly when walking and is mainly localized behind the outer ankle. Pressure pain can also be observed. Often the pain is also felt in the further course of the tendon, which is an expression of an incipient tendinitis caused by the dislocation of the peroneal tendons. Certain instabilities in the ankle also appear as symptoms, which are particularly noticeable on uneven ground. Depending on the extent and cause of the peroneal tendon dislocation, other symptoms such as bruising or overheating and reddening of the affected foot may occur.
Diagnosis
The diagnosis of peroneal tendon dislocation begins with the questioning of symptoms and the clinical examination. Palpation of the dislocated tendon and the instability to be examined by tests provide initial indications of the injury. Imaging methods can also be used in diagnostics to confirm the diagnosis and to rule out the extent and involvement of other structures in addition to the peroneal tendon dislocation. An x-ray shows bony involvement, the ultrasound can be used to visualize the tendons and examine them for tears, inflammations and dislocations. In some cases, the MRI is used.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
Athletes (joggers, soccer players, etc.) are particularly often affected by diseases of the foot. In some cases, the cause of the foot discomfort cannot be identified at first.
Therefore, the treatment of the foot (e.g. Achilles tendonitis, heel spurs, etc.) requires a lot of experience.
I focus on a wide variety of foot diseases.
The aim of every treatment is treatment without surgery with a complete recovery of performance.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
MRI for peroneal tendon dislocation
An MRI (Magnetic resonance tomograph) is used for peroneal tendon dislocation in cases of doubt, if no reliable result could be achieved with previous diagnostics, or if the structures need to be represented more precisely. For an MRI examination, lie down like a CT (Computer tomograph) into a tube, during which sectional images are made of the lower leg and foot. In contrast to CT, MRI does not show any X-rays or other dangerous radiation, and soft tissues can be assessed very well. The MRI is a highly specific and highly sensitive detection of a peroneal tendon dislocation.
Please also read our article on this MRI of the ankle.
Therapy of peroneal tendon dislocation
Conservative treatment
In recent years, the opinion of experts has increasingly been to treat peroneal tendon dislocation surgically. Nevertheless, the treatment can be conservative if there are reasons against an operation or if a better result is hoped for. Treatment conservatively is only indicated if the dislocation of the peroneal tendon is caused by an accident, for example during sports or after an ankle twist. Surgical treatment should be considered if there are genetic problems that lead to peroneal tendon dislocation. The conservative treatment mainly consists of immobilizing the affected ankle and special exercises as part of physiotherapy. In the case of acute dislocation of the peroneal tendon, immobilization is carried out using a special bandage or plaster cast that must be worn for 4-6 weeks. During this time, do not put pressure on the foot involved. However, this type of treatment of a peroneal tendon dislocation only leads to healing in about 50% of cases. At the same time, the treatment is carried out conservatively, with symptoms such as pain and swelling being treated with pain reliever and anti-inflammatory drugs (ASA, ibuprofen, diclofenac). After the plaster of paris has been removed, the patient is gradually brought up to full exercise capacity, with physiotherapy playing a decisive role after a peroneal tendon dislocation.
physical therapy
After the acute treatment of the peroneal tendon dislocation comes the phase in which the involved, atrophied muscles are rebuilt. This is done as part of physiotherapy. During physiotherapy, certain exercises are shown and performed under professional guidance, which strengthen the muscles and tendons in the leg and foot. It is usual to regain sufficient stability in about 2-3 appointments per week over a period of 2-3 months. In physiotherapy, it is important that the patient takes the tasks seriously and conscientiously carries out his training program exactly as instructed. Otherwise, the peroneal tendon can quickly become dislocated again.
OP
According to current opinion, surgical therapy should be the treatment of choice for acute peroneal tendon dislocation after an accident, and especially for constitutional peroneal tendon dislocation. Surgery is also indicated if the conservative treatment was unsuccessful. There are three different approaches: On the one hand, the peroneal tendons can be reconstructed with the help of tendons removed from another location and thus brought back to their anatomical location. However, this operation then requires a 4-8 week break in the cast. On the other hand, there is the method of transfer surgery after peroneal tendon dislocation, in which the dislocated tendons are placed under a ligament on the ankle (Calcaneofibular ligament) and fixed there. A break of several weeks is also required here. As a third option, there is a procedure in which the groove in the bone in which the peroneal tendons are located is deepened and the tendons are covered with a small, bony piece. In this deep bone groove, the tendons can slide more stable and without dislocation. The advantage here is that, depending on the pain, full weight can be exercised directly. Which surgery is used always depends on the type of peroneal tendon dislocation and the extent of the discomfort. Therefore, doctors experienced in this field should always decide on a case-by-case basis.
Prognosis, course and duration
The prognosis or the course of a peroneal tendon dislocation is consistently positive in most cases. Especially with acute, but also chronic dislocation of the peroneal tendon after optimal therapy, there is no permanent damage or restriction. Depending on the therapy chosen, it still takes several weeks to fully heal. Patients treated conservatively can usually resume full exercise after about 8 weeks of plaster and subsequent physiotherapy. The duration after surgery is similar. After reconstruction and transfer surgery, a full cast must be worn for a period of 2 weeks, and then light training can be started with a walking cast for 4 weeks. A cast is not necessary after the sulcus operation, but the load must be increased slowly. As a rule, the time until full recovery is a little shorter here. In the case of chronic dislocation of the peroneal tendon due to a weakness of the ligamentous system, the duration of the disease until the correct diagnosis can be longer, so that the prognosis is also less good.