BRCA mutation
What is a BRCA mutation?
The BRCA gene (Breast Cancer gene) codes for a tumor suppressor gene in a healthy state. This is a protein that suppresses the uncontrolled division of cells and thus prevents the cell from malignant degeneration into a tumor.
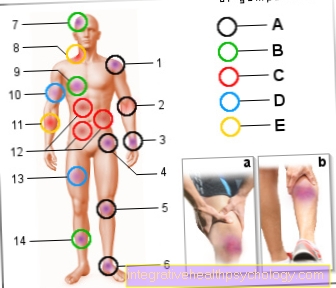
If there is a mutation in this gene, the BRCA gene carriers affected are at a significantly increased risk of developing breast cancer in the course of their lives (Breast cancer) or ovarian cancer (Ovarian cancer) to get sick.
There are two BRCA genes: BRCA1 and BRCA2. It is believed that around 5% of all breast cancers are caused by a BRCA mutation and are therefore hereditary.

What is a BRCA1 gene?
BRCA1 (Breast Cancer gene 1) is a gene from the group of tumor suppressor genes ("Tumor suppressive genes"). BRCA1 is located in the genome on chromosome 17, where it codes for proteins that protect against tumor development. The exact task of the BRCA1 gene product is to repair damage (so-called double strand breaks) in the human genome, the DNA.
Due to certain mutations, the gene may no longer function at all or only to a limited extent (Loss-of-function mutation or deletion), increasing the likelihood that the affected cell will degenerate into a malignant tumor.
For more information on this topic, see: Tumor markers in breast cancer
What is a BRCA2 gene?
BRCA2 (Breat Cancer gene 2) was discovered a few years after BRCA1. The gene is located on chromosome 13. This gene also codes in the cell for a tumor-suppressing protein that plays a crucial role in the repair of DNA damage.
Mutations in BRCA2 prevent these repair processes and thus increase the risk of certain types of cancer, especially breast and ovarian cancer.
Are you more interested in this topic? Then read our next article below: The breast cancer gene
What is the difference?
Both mutant BRCA1 and BRCA2 are both high risk genes for breast and ovarian cancer. In the intact state, the products of these genes counteract the development of tumors, although the exact function of both genes is not yet fully understood. The genes are on different chromosomes in the genome.
A mutation in BRCA1 or in BRCA2 increases the likelihood that the affected woman will develop breast cancer and the likelihood that she will develop breast cancer by the age of 70 is up to 80%.
A BCRA1 mutation also significantly increases the risk of ovarian cancer (Disease probability of 50%), whereas the risk of this disease is also increased with a BRCA2 mutation, but the probability of the disease is lower and is only 30-40%.
Can I tell from certain symptoms that I have a BRCA mutation?
A BRCA mutation does not cause symptoms that indicate the genetic change.
People with mutated BRCA genes are not sick, but they simply have a significantly higher risk of developing breast or ovarian cancer later in life.
The only evidence of hereditary breast cancer is a familial increase in breast cancer.
You can read more detailed information on this topic here: Symptoms of breast cancer
How likely are you to get breast cancer?
The majority of all breast cancers are not due to genetic changes in the BRCA genes. Studies have shown that only around 5-10% of all breast cancers are inherited through BRCA mutations. Nonetheless, women with high levels of breast cancer in their families are unsettled and wonder how likely it is that they too will develop breast cancer.
The probability for women who suffer from a mutation in BRCA 1 or BRCA 2 to develop breast cancer in the course of their further life is about 50-80% and is therefore significantly higher than that of women with non-mutated BRCA genes.
Changes in the BRCA1 or BRCA2 gene also increase the lifetime risk of ovarian cancer: women with mutations have a 50% chance of developing the disease.
Women with mutated BRCA genes also get the disease much earlier at a younger age (40 years or younger). In women with non-hereditary breast cancer, the disease does not appear on average until they are 60 years of age or later.
But not only women are affected by mutations in the BRCA genes. Men who are affected by BRCA mutations also have an increased risk of developing breast cancer during their lifetime. However, these figures only apply to so-called high-risk families, i.e. families in which several cases of breast cancer or ovarian carcinoma occurred in family members at an early age.
In addition to the two BRCA genes, there are other genes that are thought to increase the risk of hereditary breast cancer.
Are you interested in this topic? Then read our next article below: Breast cancer risk
How likely is this to be inherited?
Each gene exists in duplicate in the cell within the cell nucleus. One copy of the gene comes from the mother, the other from the father. A mutation in one of these copies is sufficient to speak of a BRCA mutation; this condition is referred to as a "heterozygous" mutation. This copy of the gene is defective from birth, whereas the second copy is still intact.
If a mutation occurs in the second copy due to environmental influences or spontaneously, the function of the gene fails completely and a "homozygous" mutation is present. As a result, the cell can no longer repair damage in the DNA and grows uncontrollably. Unchecked cell growth leads to the development of tumors.
If multiple cases of breast cancer occur in a family, it is likely that there is an increased susceptibility to the disease and that it is passed on.
The BRCA genes are inherited according to the “autosomal dominant inheritance” scheme. This means that a mutation in a BRCA gene from one parent has a 50% chance of being passed on to the children.
It is important to understand that this applies to all offspring, both female and male, and therefore the mutation can also be passed on through males within the family. On the other hand, people who do not have a mutation in the BRCA genes do not pass on any BRCA mutations to their children, as gene changes are only passed on directly to the offspring and cannot skip a generation.
If you're more interested in this topic, then check out our next article below: Is Breast Cancer Hereditary?
These tests are there
A genetic test is carried out in the laboratory, in which a blood sample is examined for mutations in the BRCA1 and BRCA2 genes.
A genetic test is a molecular biological test in which the genetic material is analyzed.
For women who are considered to have a family history with regard to breast and / or ovarian cancer, the costs for this genetic test are usually covered by the health insurance company.
The test results are so certain
The examinations provide reliable results, but the evaluation of the test results is often not easy.
In addition to the mutations that significantly increase a patient's risk of developing breast or ovarian cancer, there are also neutral changes in the BRCA genes. These are also mutations, but they have no effect on the risk of cancer.
It is not always easy to distinguish between disease-relevant and neutral changes, which is why not every finding can be assessed with absolute certainty.
Who should be tested?
Women with a family history should be tested for a mutation in the BRCA genes. This includes people who come from a high-risk family. There are certain criteria that must be met for this. You can find these in our article: Genetic testing
For example, at least three cases of breast cancer in the family, at least two women with breast cancer before the age of 51, at least one man with breast cancer, or at least two women with ovarian cancer.
A genetic examination only takes place after the age of 18, as cancer almost never occurs in very young women.
What is the treatment for a BRCA mutation?
Women who have been found to have a mutation in BRCA1 or BRCA2 should speak to their doctor about their risk of developing breast and ovarian cancer and about possible prophylactic treatment.
However, a positive genetic test does not mean that cancer is already present, nor that this will inevitably happen. Existing mutations in the BRCA genes can only be an indication that the disease risk for breast and ovarian cancer over the entire lifetime is significantly increased compared to people without a mutation.
A BRCA mutation cannot be treated per se. However, women with positive results should take part in an intensified early detection program. The doctor carries out regular preventive examinations in order to be able to detect a possible breast or ovarian cancer as early as possible. Cancer that is diagnosed and treated at a very early stage has a very good chance of recovery.
The early detection program includes a six-monthly palpation examination and an ultrasound examination of the mammary glands. In addition, a mammography is performed annually from a patient age of 30 years.
Alternatively, there is also the option of a preventive operation, in which both breasts, the ovaries and fallopian tubes are preventively removed. This operation is a very radical measure that needs to be carefully considered. Affected women have the opportunity to discuss this decision in detail with a team of experienced gynecologists and human genetics.
Psychological support is also part of the treatment, as the situation is an enormous psychological burden for many patients. After a breast removal, there are a number of possibilities to reconstruct the removed breasts as lifelike as possible.
You can read more information on this topic: Therapy for breast cancer
How can one make the diagnosis?
A BRCA mutation is diagnosed using a genetic test in which the two genes are examined using genetic diagnostics. A genetic test only makes sense if a person is likely to have a hereditary predisposition due to a family history of breast or ovarian cancer.
A blood sample is taken from the test person, from which the DNA, i.e. the genetic material, is obtained. The actual investigation is carried out by means of gene sequencing. Certain gene segments in which the mutations can be located are completely sequenced. This means that the individual DNA building blocks are deciphered and examined.
Due to the complex examination technology, it can take up to four months before the final test result is available.
Are you interested in this topic? Read more about this under: How do you recognize breast cancer?
What is the prognosis?
The prognosis for women with a BRCA1 or BRCA2 mutation depends largely on the treatment initiated.
Regular checks as part of an early detection program significantly improve the prognosis, as possible tumors can be detected very early and treated well.
The actual prognosis for breast cancer is no worse for women with the BRCA mutation than for other patients with non-inherited breast cancer.
Are you interested in this topic? Read our next article below: Prognosis in breast cancer
Causes of a BRCA mutation
Mutations are constantly developing in our body cells, but these are usually quickly repaired by special mechanisms and therefore have no consequences for the organism. A multitude of external influences can trigger mutations and disrupt the function of a gene. The triggering factors are called mutagens.
These possible causes include, for example, high-energy radiation (e.g. X-ray or UV radiation), various chemicals (e.g. Nitrosamines and polycyclic aromatic hydrocarbons). In retrospect, however, it is difficult or impossible to determine a specific cause for the mutation.
Special mutagens that primarily cause mutations in the BRCA genes are not yet known. In most cases, mutations in the BRCA genes arise simply by chance anyway (so-called spontaneous gene mutations).
This is where errors occur during the DNA doubling as part of cell division, which changes the gene. As a result, there may be problems with cell growth, which increases the risk that a malignant tumor will develop in the further course.
Psyche with BRCA mutation
The suspicion of a BRCA mutation or a positive genetic test represents a considerable psychological burden for the patient that should not be underestimated. For this reason, many clinics where the genetic analysis is carried out offer detailed consultations, which also include a conversation with a psychologist.
The decision as to whether the breasts and ovaries should be removed as a precaution before tumors can develop is also a psychological challenge and, in addition to thorough advice, requires a special psychological examination.
Studies have shown that mental illnesses such as depression or extreme stress are risk factors for breast cancer and can promote tumor development. For this reason, it is particularly important that genetically pre-stressed women receive appropriate psychological support in order to strengthen their positive attitude towards life and their psychological well-being.
This topic may be helpful to you: Postoperative Depression
Which other tumors are associated with a BRCA mutation?
The BRCA genes encode proteins that normally prevent the cell from growing excessively and dividing uncontrollably. Changes in these genes mean that this is no longer guaranteed and cancer develops.
These are preferably tumors that are located in the breast or the ovaries, but there are also other cancers that are associated with a BRCA mutation. These include intestinal, pancreatic (pancreas-) and skin cancer. Men also have an increased risk of prostate cancer.
You can read more information on this topic: Skin cancer - early detection and treatment
What is the connection between the BRCA mutation and ovarian cancer?
There is also a link between changes in the BRCA genes and inherited ovarian cancer. Women with a mutation in the BRCA1 or BRCA2 gene have an increased risk of breast cancer and a higher probability of developing ovarian cancer.
It is estimated that carriers of mutated BRCA genes have a 50 percent risk of ovarian cancer later in life.It is also possible that carriers of BRCA mutations develop breast and ovarian cancer in parallel.
In contrast to breast cancer, there is unfortunately no proper early detection program for ovarian cancer. Nevertheless, the doctor can regularly examine the ovaries for tumor-suspicious masses using ultrasound.
Women who tested positive should also think about a preventive operation that involves removing the fallopian tubes and ovaries in addition to the breasts. Of course, this is not an easy decision and depends largely on the life situation (Age, completed family planning, etc.) from. Therefore, this step should be carefully considered and discussed in detail with the treating physician.
You can read more detailed information on this topic here: Ovarian Cancer - Symptoms, Causes and Treatment
What does triple negative actually mean?
Triple negative or triple negative breast cancer is a special form of breast cancer that is negative for three specific markers.
The estrogen receptor (HE), the progesterone receptor (PR) and the human epidermal growth factor receptor 2 (HER2).
These receptors can exist on the surface of the tumor cells and ensure that the tumor responds to certain hormones (estrogen, progesterone and the epidermal growth factor) addresses what affects the treatment regimen.
This is not the case in the case of a triple negative carcinoma. It has been shown that women with triple negative breast cancer often have a mutation in BRCA1.
Are you interested in this topic? Then read our next article below: What is triple negative breast cancer?
Recommendations from the editorial team
Further general information on the subject of "BCRA mutation":
- How can you detect breast cancer early?
- Hormone therapy for breast cancer
- Tumor markers in breast cancer
- How can you feel breast cancer?
- Breast cancer recurrence
- Genetic test





.jpg)